In the last few years, a new type of financial consolidation has caught the attention of antitrust regulators. Institutional investors—big companies like Fidelity and BlackRock—today own 70 percent of publicly traded stocks, according to some estimates, which means that one big investor could own significant shares of the companies that nominally compete within the same industry. Two 2016 studies found that this relationship may have had a causal effect that produced higher prices for consumers in the airline and banking industries. Now a new analysis published in Health Affairs finds that this type of informal consolidation among investor-owners has nearly doubled in at least one sector of the healthcare industry during the last decade. Between 2005 and 2015, the percentage of acute-care hospitals that share significant ownership with post-acute facilities and hospices grew from 24.6 to 48.9 percent.
Earlier studies of consolidation in healthcare, says lead author Annabelle Fowler, a Ph.D. candidate in health policy at Harvard Medical School (HMS), have focused on formal mergers—what people typically imagine when they think of companies exercising monopoly power. “We wanted to peel away that layer and see who the underlying investors are, and [ask if] there are any ties across these sectors that we might not be able to immediately see, but that might have implications for the care people receive.” The team focused on common ownership of acute and post-acute facilities, Fowler explains, because post-acute care is the source of a lot of variation in Medicare spending; financial consolidation, the researchers speculated, might be a potential explanation.
The group (including co-authors David Grabowski and Haiden Huskamp, professors of health care policy at HMS, and Robert Gambrel and David Stevenson of Vanderbilt) pulled their data from the Provider Enrollment, Chain, and Ownership System (PECOS): a database of every medical provider in Medicare, with granular information about every investor owning a 5 percent or greater share in each provider (though it doesn’t show how large a share the investors hold—only that it’s at least 5 percent). “What’s really novel about this paper is the use of this dataset,” Fowler notes.
The team considered only institutional investors in their analysis. They then looked at the financial links between healthcare providers within the same region—a hospital and a skilled nursing facility (a type of long-term, post-acute-care provider) in a single state, for example. An investor with shares in a hospital in Boston and skilled-nursing facilities in Seattle, for example, wouldn’t count as common ownership under their rubric.
The findings are striking: the percentage of hospitals with a link to other healthcare facilities (including acute-care hospitals, skilled-nursing facilities, home health agencies, long-term care hospitals, inpatient rehabilitation facilities, and hospice agencies) via a common owner almost doubled during the study period. That might be in part because the share of healthcare providers with any corporate investor increased significantly during the same period (from just over one-quarter to more than one-half), across each of the six types of facilities studied. In other words, corporate investors’ share of providers has simply increased over time, just as it has in the economy overall. “Our results have potential implications for how we think about competition between and across sectors,” says Grabowski. “If an investor jointly owns several hospitals within a market, are these hospitals really competing with one another on cost and quality?”
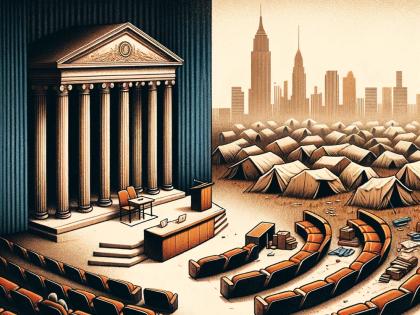
What might this mean for regulators? Common investor ownership, unlike formal mergers, is not currently regulated, but can be deemed illegal if the behavior of investors is construed to produce collusion among different companies. The analysis doesn’t claim a causal relationship between common ownership and the quality or cost of healthcare, but financial consolidation across the industry can create anti-competitive incentives that are bad for patients.
“If you’re a particularly expensive patient,” Fowler explains, “then the hospital might [have an incentive to] refer you to a skilled-nursing facility that’s not under common ownership, because you’re sort of a burden. If you’re a patient with less risk, then a doctor might have incentive to refer you to a provider within the same common ownership.”
It’s not clear how a financial link between healthcare facilities could translate into this sort of decisionmaking at the level of individual doctors. But investors can influence companies in many ways—for example, through their votes on business decisions at shareholder meetings. Much work remains to be done, by academics as well as regulators, on the dynamic between investors and industry competition. At a minimum, Fowler and Grabowski suggest that there is a need for more transparency in these relationships; mandated disclosure of large-scale common investors could be the best next step. That would benefit not just researchers and regulators, Grabowski says, but patients as well. Both groups, presumably, would want to know if there is any investor linkage among healthcare providers.