During his first year as a neurology resident, Michael P.H. Stanley ’13 was paged to the room of a delirious patient. The terminally ill man, agitated and defiant, had gotten out of bed, taken off his hospital gown, and was packing his suitcase to go home. He couldn’t speak, because of the aperture in his throat made by a tracheotomy, but the nurses told Stanley that he had been writing “nonsense” messages to them all night. Stanley asked the man why he was trying to leave the hospital, when he’d be released anyway in the morning, into hospice care. On the back of an envelope, in all-caps, the man answered, “Tomorrow creeps in this petty pace.” Stanley lit up. This wasn’t nonsense, he realized. “It’s Shakespeare!” Reciting the rest of the soliloquy from Macbeth—which ends with those famous lines about a tale “full of sound and fury, signifying nothing”—Stanley tucked the patient, now calmer, back into bed.
In an essay he published about the episode in the Wall Street Journal a few months later, in June 2019, Stanley mused about how that quote, which the patient had memorized for perhaps some long-ago school performance, had resurfaced “to express his anguish and confusion” at a moment “when his own words faltered.” “It was a cry to be heard as a human being,” Stanley wrote, “and I was on call to hear him.”
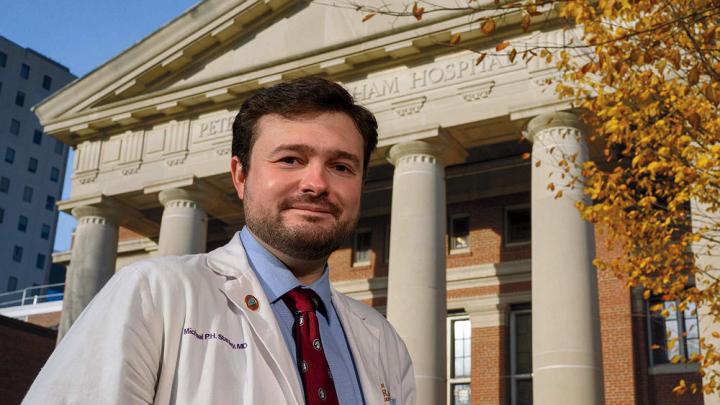
Recalling the story more recently, sitting on a park bench outside Brigham and Women’s Hospital, where he’s now a third-year Harvard Medical School resident, Stanley was still thinking about that last part: the humanness on both sides of the medical encounter, and the importance of remaining open to it. A writer as well as a doctor, he has a growing portfolio of published dispatches from the medical wards, most revolving around some aspect of that central idea. “My fight right now is to not become a tradesman,” he says. He acknowledges there’s good reason for checklists and standardization in medicine—“for thinking of us more like pilots”—but he sees limits to that approach, too. After all, health care is an industry, and “if we let it, it will make machines out of us.”
By contrast, medicine is a profession, he says, more like a covenant than a contract. “Doctoring,” Stanley calls it: “You get the privilege of meeting people in some of the most beautiful or strange or horrible parts of their lives.” And it’s important to remember, “Every patient is an N of 1,” he says, borrowing the term for a clinical trial in which a single patient is the only subject.
The turning point Stanley remembers as a “Damascus moment,” when he decided all at once to become a neurologist, came during his sophomore year at Harvard. Gary Sullivan, a family friend with amyotrophic lateral sclerosis (ALS), was traveling to Boston for a day of appointments at the ALS clinic at Massachusetts General Hospital, and he invited Stanley along. During the clinical exam, Dorn professor of neurology Merit Cudkowicz showed Stanley how to use a reflex hammer on Sullivan’s knee and to feel for muscle tone. “To me, it was like remote viewing, like trying to find a spy behind enemy lines,” he says. “Because you can’t interrogate the nervous system directly, right? It’s all through shadow and effect.” His own exams now, he jokes, look like “either a magic show or a clown show,” with him asking patients to tap their feet and touch their noses and draw pictures of bicycles. “But all these little things—we’re looking to see where there’s a breakdown in the nervous system.”
That day in Cudkowicz’s office was a revelation for Stanley. “I saw this overwhelming ability to detect a problem, mind to mind, hand to hand, strength to strength. It was beautiful.” The visit wasn’t gloomy or fatalistic. Sullivan and Cudcowicz talked about orthotics to help him walk better in the woods, and lighter sheets to help him to turn over in bed. That summer, Stanley began working with Cudcowicz on ALS research.
Before then, his interests might have taken him in almost any direction. Stanley grew up in Springvale, a mill town in southern Maine, where 11 generations of his family have lived, occupying the same core plot of land since the early 1700s. His father is president of the local chamber of commerce and his mother worked as a family and real-estate attorney. For Stanley and his sister, the house was full of books and poetry and music. He played piano well enough to perform at restaurants for gas money and thought briefly about music school. Family friends included an English teacher who recited Robert Service poems—“those were our campfire stories”—and a burly outdoorsman who was “the closest guy I’ve ever met to Falstaff,” Stanley says. “He had a compendium of Shakespeare quotes and Spaghetti Western quotes, and he could just blend one into the other.”
As an undergraduate, Stanley did his best to exhaust either himself or Harvard. His concentration was human developmental and regenerative biology, but he also studied politics, literature, and ancient philosophy. He took classes at the Divinity School, the Business School, and the School of Public Health. “There was a fire burning in that kid,” recalls Gail O’Keefe, former faculty dean at Eliot House, where Stanley lived for three years. As a senior, he won a Finley Fellowship and his itinerary included stops in Australia, South Africa, and Scotland, where he retraced the traveling routes of eighteenth-century writer Samuel Johnson, whose work he’d come to revere during a seminar the previous year (one favorite quote, among many: “There has rarely passed a life of which a judicious and faithful narrative would not be useful”). In England, he paid a side visit to Edward Stanley, the nineteenth Earl of Derby, with whom he shares a common ancestry. “I wrote to him and said, ‘You know, it’s been 400 years since our Stanleys have seen anything of the English Stanleys, and I would like to meet you.’” The earl’s answer: “‘Absolutely.’”
That exchange doesn’t surprise O’Keefe, who remembers Stanley as ardently immersed in Eliot House social life, seeking out the company not only of fellow bookworms, but also of the club kids and partiers, and of O’Keefe and her husband, Douglas Melton, Xander University Professor and co-director of the Harvard Stem Cell Institute. “For his friends and blockmates, he would do things like hand-tie fishing flies to give for their birthdays,” she says. At graduation, he made a letterpress print of a poem he’d written and framed as a parting gift for her and Melton. As a graduation gift to himself, he collected pencils from each of the Harvard libraries. “He’s just such an old soul,” O’Keefe says. “He’s one of those people who really honors his connections.”
After college, Stanley attended Tufts Medical School, where he enrolled in the Maine Track Program, which allows students interested in rural medicine to spend two years working at clinical sites throughout Maine. He trained with internist Richard Kahn at Pen Bay Medical Center, a 99-bed community hospital in coastal Rockport. “Good common sense and empathy,” is how Kahn describes Stanley’s bedside manner. But the two men really came together over their shared interests in humanities and medical history. In 2016, when Stanley arrived, Kahn was close to finishing a 30-year book project on the life and writings of a doctor practicing just after the Revolutionary War—published in 2020 as Diseases in the District of Maine 1772-1820: The Unpublished Work of Jeremiah Baker, a Rural Physician in New England (Oxford University Press). Working with Kahn to publish historical pieces of his own, Stanley began to think of himself as a writer.
These days, amid 80-hour workweeks as a medical resident, Stanley writes occasionally about his experiences in the hospital, trying to capture moments that are instructive or revelatory. In another Wall Street Journal essay from 2019, he wrote about a 90-year-old minister given the sudden and unexpected responsibility of serving as health-care proxy for a dying member of his congregation. Last August in the culture and philosophy magazine Aeon, Stanley told the story of an artist who suffered from atypical Parkinsonism, a syndrome that stiffened her movements and eventually brought on dementia. He chronicled her disease’s progression through her artwork, as hallucinations increasingly occupied her canvas, and as she switched from using a paintbrush to a palette knife, and finally to collage, a format in which, he wrote, “meaning manifests as a whole from broken pieces and fragmented ideas.”
More recently, he’s been working on an essay about a stroke patient who temporarily developed an “alien hand,” whose behavior was not under her control. “And these are not just odd movements,” he says. “It would do thoughtful things”: grab a cup, unbutton a shirt, sometimes try to hit people. He remembers the patient saying of the hand, which she called “he,” to dissociate it from herself: “When I get anxious, he gets angry.” As her stroke symptoms receded, so did the alien hand, “but now she lives with this undercurrent of fear that anytime she drops something or gets tingly—is he coming back?” Stanley says. “She taught me something about how little we think about what makes us who we are,” and how easily susceptible the self is to alteration, in ways that are often unpredictable.
Stanley frequently brings ideas from philosophy, history, and literature into his meditations on neurology.
Stanley frequently brings ideas from philosophy, history, and literature into his meditations on neurology. Ask him a question about dementia or multiple sclerosis, and his answer might begin with the origin of the stethoscope, or the preacher in Marilynne Robinson’s novel Gilead, or a line from poet Philip Larkin. Lately, he’s been reading Umberto Eco’s research on symbols and art historians Ernst Gombrich and Aby Warburg on Warburg’s study of Hopi snake-dance rituals, all of which has Stanley thinking about gesture as a form of language and cognition, and as a bridge between physical and metaphysical understanding. “For people with language disorders, do their gestures change?” he wonders. “What about people with thought disorders?” Questions like these alter how he examines patients, he says, and the attention he pays to phenomena that might otherwise seem insignificant. “Michael’s going to be a good neurologist,” says Martin Samuels, Joseph Distinguished Professor of neurology and founding chair emeritus of Brigham’s neurology department. “You have to be interested in cognitive work, work that is mostly thinking. Michael likes to think about the causes of things, the philosophical relationships, the history.”
When the pandemic hit, Stanley wrote about that too, looking again for glimmers of human connection and mutual vulnerability amid the crisis, contemplating its effects on his own practice and patients. By August 2020, he was arguing in the National Review that COVID-19 was not our Pearl Harbor, as some labeled it, but “our Somme”—a long, bloody slog like the World War I battle that stands as the grim epitome of trench warfare.
And lately, he’s been involved in a project that feels like an extension of his writing: working with the Annals of Neurology and two medical organizations—the Boston Society of Neurology, Neurosurgery, and Psychiatry and the American Osler Society—to help bring new, younger members into their fold. (Stanley feels particularly invested in the humanistic mission of the Osler Society, named for doctor, scientist, and medical educator William Osler.) The effort is just beginning, but so far Stanley has been planning podcasts and essays, working to build mentorship networks, and soliciting other physicians to share their written stories, articles, or webinars with him and each other. “We’ve got a home for you here,” he tells them. It’s a project he feels deeply about, in a way that goes back to the humanness of medical practice, doctors’ need for community, and the importance of resisting the mechanization of caregiving and caregivers. As with his writing and his doctoring, Stanley says, “It’s about trying to build back a society, lowercase-s.”