It's a troubling area, the economics of saving lives. Take cervical cancer, for example. In the United States we have spent enormous sums for the prevention and treatment of the disease and have evenunlike the case with most cancerslearned what causes it: the sexually transmitted human papillomavirus, or HPV. In the last 40 years, the incidence of the disease has declined by 80 percent in this country, due largely to aggressive screening for its precursors. Cervical cancer is now one of the less-fatal cancers for American women.
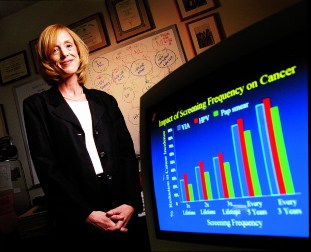 |
| Deploying computer models rather than clinical trials, Goldie identifies life- and cost-saving strategies to detect cancer. |
| Photograph by Jim Harrison |
It's a different story in the developing world. In a stark example of international healthcare disparities, cervical cancer is the third most common cancer worldwide, and the leading cause of cancer death among women in some poor countries. Each year, 466,000 new cases develop80 to 90 percent of them in developing countries, with rates highest in sub-Saharan Africa and Central America. Nearly 200,000 women in developing countries die from the disease annually.
They die because, typically, no one screens them for the cancer's precursors. The American screening methodthe Papanicolaou (Pap) smearis difficult to administer and beyond the budgets of impoverished nations. Instead, up to 80 percent of those afflicted learn they have the disease only after it has reached an advanced stage, when their deaths are virtually assured.
In sub-Saharan Africa, cervical cancer deaths take an especially high social toll: many victims are women who have reached their late thirtiesthe age at which most cervical cancers developwithout becoming carriers of HIV. These women are caring for their own children and the children of women who have died of AIDS. Their value in their communities is great.
Many of them could quite easily be saved, despite their countries' meager resources. That's the conclusion of Sue Goldie, M.D., M.P.H '97, assistant professor of health policy and health decision science at the School of Public Health (SPH). Through research in South Africa, Goldie has found that inexpensive screening and treatment strategiesalternatives to Pap smearscould prevent up to one-third of cervical cancer cases there. Her findings, she says, could likely be applied in other impoverished settings. Now she wants developing nations and international aid organizations to know that such options are available.
 |  |
| Above: At the women's clinic of Clinique Bon Saveur in rural Haitithe poorest, most health-deprived country in the Western Hemispherewhere Goldie begins a screening program in August. Above right: The clinic in Khayelitsha, South Africa, where Goldie developed her model, and rudimentary cryosurgery gear. |  |
| Photographs courtesy of Sue Goldie | |
Goldie, who calls herself a "heart-and-soul doctor" and also a "closet geek," is passionate about the ability of quantitative analysis to save lives. Having left the regular practice of medicine four years ago, she now conducts research using the methods of a discipline called decision science, a rigorous approach to decisionmaking under conditions of uncertainty. The field has provided her with a way to combine her concern for patients with her bent for numbers: the discipline applies a collection of quantitative, analytic toolsincorporating elements of economics, statistics, and psychologyto complex real-world problems. In the last two decades its methods have been used in public health to study everything from the costs and benefits of automobile airbags to strategies for controlling global warming. Goldie builds mathematical models to study the patterns of infectious diseases and discover effective approaches to preventing and curing them.
For her research on cervical cancer in South Africa (funded by the Bill and Melinda Gates Foundation), Goldie and her team of researchers from universities in the United States and South Africa reviewed previous studies and gathered data on the natural history of the cancer there; on the effectiveness and cost of various screening and treatment strategies; on the prevalence and types of cervical cancer found in the population; and on factors such as age, income, and HIV status. Using these data, they built a mathematical model that represented the at-risk population and the disease. They tested the model's validity by entering historical data and verifying its ability to predict present-day numbers. Once the model proved sound, Goldie tested five potential screening and treatment strategies, ranging from a simple, once-in-a-lifetime visual screening to more frequent laboratory Pap screens. The data are real, but the testing is "virtual": it happens not on people but on numbers in a computer, which uses algorithms to determine outcomes for each strategy, applying the gathered data.
The "beauty of the modeling methods," Goldie says, "is that, unlike clinical trials, they do not pose the ethical problem of offering potentially beneficial treatments to only one portion of a population." In other words, because the computer closely mimics the "real world," there's no need to treat real humans as guinea pigs. But Goldie emphasizes that modeling is not better than a clinical trialit simply uses different methods and fulfills a different purpose. Unlike clinical studiesin which limited alternatives are tested under controlled circumstancesdecision science seeks to address all relevant, real-world variables: such factors as the likelihood of power outages, the scarcity of doctors, or how far from the clinic women live. Goldie's research did not "control" for such differences, but deliberately sought to include them.
The study also departed from traditional clinical trials in its examination of several screenings and treatments. "With clinical studies, usually only two alternatives can be looked at. But decision science incorporates every possibility," Goldie says. "You're not allowed to look at one thing in isolation." The discipline is also "action-oriented," she says: "You want the answer to a problem because you want to do something. You're not looking for 'the truth' so much as you're looking for the best action given the circumstances." There may not be any absolutely right answers. Goldie calls this uncertainty and complexity "messiness," and she loves working with it. She also finds herself driven to take steps away from pure research and toward advocacy, to help health policymakers arrive at the best strategy for attacking a problem, given its particularand messycircumstances.
One central issue is cost-effectiveness: how much benefit does a healthcare strategy offer for its price? The subject can raise vexing questions about access and equitable care, about how much societies can or are willing to spend to save lives. The recommended U.S. strategyannual Pap smears with subsequent visits, when necessary, for further diagnosis and treatmentcarries an average lifetime cost of $2,520 per woman. Athough enormously expensive, the strategy reduces the cervical cancer rate by 86 percent when compared with not screening at all. (Earlier this year, a panel of medical experts changed the standard recommendation to a Pap smear every three years. The change is expected to lower costs without sacrificing effectiveness.)
Compared with strategies that Goldie tested using South African data, the traditional U.S. method ranks low in simple cost-effectiveness terms. One South African strategy carried an estimated average lifetime cost of $41 per woman, and reduced the incidence of cervical cancer in the population by one-third. That strategy uses automated DNA screening to test women just once in their lifetimes for the carcinogenic HPV virus. During the same single visit, women with suspected precancerous lesions receive cryosurgerythe freezing of abnormal tissue with liquid nitrous oxide or carbon dioxide. Another strategy carried an estimated average lifetime cost of just $39 and reduced cervical cancer by one-quarter. The simple procedure is again performed only once in a woman's lifetime: a nurse or midwife applies vinegar to the cervix and examines it with her naked eye. Certain whitening of the tissue indicates precancerous cells. As with DNA testing, the strategy requires following the screening with immediate cryosurgery when necessary.
Still, as every HMO patient knows, greater cost-effectiveness does not necessarily mean better care. The U.S. method, though less cost-effective, saves more lives; African cervical cancer rates would not fall to the levels found in the United States even with the dramatic improvements Goldie's proposed strategies seem to offer. After she released her South African findings, some who work with the disadvantaged in developing countries criticized the project as advocating lesser care for poor women. Others, mostly researchers, urged further study, wanting clinical, "real-world" proof, beyond modeling, that the alternative screening methods work. "But doing nothing is a strategy also," Goldie says. "It has consequences. Arguing for another year to consider the issue means another 25,000 lives lost. It's unforgivable."
 | |
| Above: Patients queue for appointments at Clinique Bon Saveur. Right: Mother and child awaiting care in Haiti | 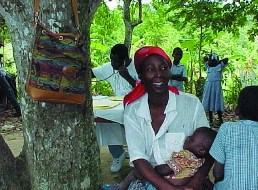 |
 |
| Goldie and young girls during a recent visit to the Haitian clinic. |
| Photographs courtesy of Sue Goldie |
Goldie is a plain-speaking, kinetic woman, no one-dimensional number-cruncher. She holds a third-degree black belt in tae kwon do, and once had to decide whether to train for the 1988 Olympics, or go to medical school. She chose school. Now she manages, with the help of a ready sense of humor, to be a researcher, the mother of two young sons, and the wife of a busy physician. During whatever free time she finds she practices tae kwon do or switches to the fine artssketching with charcoal and pencil. "What I do well in drawing," she says, "is capture people's emotions, especially children's, on paper."
She believes that multifacetedness is one of her greatest professional strengths. Her training as both a physician and a public-health researcherand her ability to speak the language of eachhas helped her to bridge the worlds of clinical care and policymaking. For example, she has tried to persuade the World Bank to include cervical-cancer screening in its reproductive-health budgets. "I see part of my role," she says, "as explaining scientific results to policymakers and encouraging them simply to consider available clinical options." Without resorting to some degree of advocacy, she feels, "Nothing will get done." She measures her success in large part by the increased debate she's witnessed around the issue of cervical-cancer screening"the real precedent for change and action."
Her drive to help solve complex health problems, rather than treat individual cases, spurred Goldie along an adventurous path to her current work. Eight years ago, following her own residency at Yale, she was caring for AIDS patients at a New Haven hospital and helping to direct a training program for residents. Stanford University invited her to join a faculty-development program: a study of how doctorsin this case, Goldie and four otherstaught medical decisionmaking. During the course of the six-week program, she says, she got hooked on decision science: "I was falling in love with the stuff we were practicing teaching. I loved bringing the scientific method to all these variables, under conditions of uncertainty." She remembers flying back across the country after the workshop and "deciding that this was it. I was going to find someone who did decision science to study with."
That turned out to be Milton Weinstein, Kaiser professor of health policy and management and biostatistics at SPH. Even though enrollment had officially closed for the year, Goldie talked her way into the program. Three nights a week for the next two years, she rode the "mail train"it left at 2 a.m. with herself, the conductor, and sacks of mailfrom New Haven to Boston. She unlocked a bike she kept chained to a fence in Back Bay, pedaled her way in the gray light up Huntington Avenue, and took classes at the Harvard Center for Risk Analysis, SPH's center for decision science. (She continued, meanwhile, to care for patients in New Haven.) Eventually she and her family moved to Boston and she found a teaching job at SPH, where her research focuses on sexually transmitted diseases, including HPV and HIV, and on hepatitis C.
Goldie says she spends "100 percent of my time on research, and a good deal more on top of that on teaching." In the past, she's had more difficulty finding funds for her research in the developing world than for research in this country, and says she has often had to limit her work on the problems of poor countries to weekends. But that pattern may be changing: the National Institutes of Health and the Gates Foundation have awarded Goldie and her team grants to expand their cervical-cancer research to Thailand, Peru, and other developing countries, and to set up screening programs based on their findings.
Follow-up data from these efforts will demonstrate the real-world effectiveness of her research findings. This means that eventually Goldie will learn how many real lives the methods have saved, at least in the short term. The first of the projects starts this August, when she'll help to screen 1,000 women in Haiti. Within the next three years, she and her colleagues plan to have screened all women between the ages of 30 and 60 in one region of rural Haiti. To her, the work is urgent. "There's a 15-year window in women's lifetimes in which we can prevent or cure many cases of this disease, out-of-doors, with one screening by a midwife with a few weeks training," she says. "How can we afford not to do at least that?"
Nell Lake is a freelance writer who lives in Belmont, Massachusetts.