Driven to Cure
Driven to Cure
Stephen B. Howell Photomontage by Bartek Malysa On a breezy San Diego evening, Stephen B. Howell, M.D. '70, dons his white coat and begins...
Stephen B. Howell Photomontage by Bartek Malysa On a breezy San Diego evening, Stephen B. Howell, M.D. '70, dons his white coat and begins scanning notes on a patient suffering from cancer of the brain and spinal fluid who has also developed a bad case of pneumonia. He enters the man's room with a hearty "Top of the evening to you." The 41-year-old patient, a Jamaican, is propped up by a mound of pillows. Though weak, he seems cheered by the doctor's attention. Howell listens to the man's chest and taps his sinus cavities. A biopsy is scheduled. "The important thing is that you are getting better," Howell tells the man. "But we would like to know what caused this in the first place, so it doesn't happen again." As an oncologist at the University of California San Diego [UCSD] Medical Center, Howell sees patients at the beginning and end of each day. He confronts the human face of lymphomatous meningitis, the still mysterious, potentially fatal form of cancer that invades the brain's protective covering, is impervious to standard chemotherapy treatments, and affects more than 6,000 people a year. Such clinical work might be enough for many physicians. But in between daily rounds, Howell transforms himself from doctor to ground-breaking scientist. The wiry 53-year-old cancer researcher has co-invented a new device--a kind of foam with the consistency of skim milk--that can carry medication against cancer, and potentially against other diseases as well. "We're interested in getting drugs to tumors and getting them to stay there for a long time," Howell says during a conversation at his medical-school office. "Before, we weren't able to get the drugs to these [brain infection] sites, because the blood-brain barrier is designed to protect it." In March, after years of clinical trials and more than a few bumpy production cycles, the U.S. Food and Drug Administration approved a system using the new technique, DepoFoam, in what is now the agency's only approved treatment for lymphomatous meningitis. Howell has always been interested in finding new methods for treating cancer that focus on patients' overall well-being, not just on the defective cells inside their bodies. In the early 1980s, he came up with a new way to treat ovarian tumors. Instead of injecting patients with drugs intravenously and risking toxic side effects throughout the body, he figured out a way to inject drugs into the tumors directly, through a stomach catheter--the first time such a treatment had been successful. (In 1989 his efforts against ovarian cancer earned him the Milken Family Medical Foundation Award.) In 1985, Howell and a former postdoctoral researcher, Sinil Kim, came up with the idea of biodegradable foam that could deliver a month-long dose of drugs to a tumor site. They spent several years testing and retesting the material before perfecting the product, which has a honeycomb-like structure of tiny chambers, each about the size of a red blood cell and each containing a specially formulated, sustained-release dose of the anticancer drug cytarabine. Over time, the foam's chambers break down and release the drug directly to the tumor. DepoFoam not only allows physicians to administer a smaller dose of medication, thereby reducing potentially harmful side effects, but also extends the dosing interval to once every two weeks, instead of two doses each week. "We were breaking new ground," Howell recounts. "There were no recipes for how to structure the spheres, how to get the drug into the spheres, or how to make the formulation stable." Howell routinely works 80- to 90-hour weeks, often skipping meals to attend lectures or draft grant proposals. Weekends are no excuse for down time. As director of UCSD's cancer pharmacology program, he runs two research labs: one tests for more effective ways of delivering drugs to infection and tumor sites, and the other looks at the genetics of cancer-drug resistance. He also cofounded, and now advises, DepoTech, a biotechnology firm that develops applications for DepoFoam. (The company, purchased by British pharmaceutical-maker SkyePharma in 1999, recently started testing the foam as a way to deliver morphine directly to the body's pain receptors. That would allow patients to use morphine as a local anesthetic and avoid circulating the narcotic painkiller throughout the body. Clinical trials are also being held to test the foam's effectiveness with amikacin, a "broad-spectrum" antibiotic used to treat serious infections.) Howell admits that his intense work schedule has long been the subject of family discussions. "I don't think anybody works as much as he does," says his wife, Julianne Reich Howell '67, A.M. '68, M.P.P. '77, Ph.D. '80, herself director of strategic planning for UCSD's burgeoning medical center. The couple met while both were studying at Harvard Medical School's Countway Library and married a year later in Appleton Chapel at Memorial Church. While he pursued advanced training in oncology at Dana-Farber Cancer Institute and the National Institutes of Health, she worked on her dissertation for the Kennedy School. Three years after he became, in 1977, one of the founding faculty members at UCSD's cancer center, she took the job she still holds. Howell points to their sons, Justin '01 and Brett, now studying psychology at the University of Miami, as proof that he and his wife haven't sacrificed family for their careers. "They are doing dynamic and interesting things," he says. "If you measure us by the outcome, by the parenting job, we seem to have survived the process." Family vacations in New Hampshire, throughout the West, and overseas have been a tradition ever since the couple spent six months studying tropical diseases in the Caribbean and took their young boys along. "I like to work hard and play hard," Howell explains. Every summer, he and a group of friends board inflatable rafts for several weeks and navigate some of the West's most challenging waterways, such as the Grand Canyon section of the Colorado River or the Salmon River in Idaho. "It's a terrific way of relaxing and getting away from it all," he says. But once back at the medical center, he continues, "You get fascinated by the problems you are working on. And if I'm going to do something for people with this terrible disease, I don't have a long time to do it." Being a doctor and a scientist is a major challenge, he acknowledges. "But by focusing on the key issues--knowing where I think I can make a contribution--I'm able to sustain both." ~Eric Niiler Eric Niiler is a freelance writer and a correspondent for KPBS public radio in San Diego.
Explore More From Current Issue

For Campus Speech, Civility is a Cultural Practice
A former Harvard College dean reviews Princeton President Christopher Eisgruber’s book Terms of Respect.
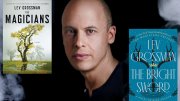
Novelist Lev Grossman on Why Fantasy Isn’t About Escapism
The Magicians author discusses his influences, from Harvard to King Arthur to Tolkien.
Getting to Mars (for Real)
Humans have been dreaming of living on the Red Planet for decades. Harvard researchers are on the case.