By the time he reached his early thirties, James was a promising scientist who had all the makings of an academic star. He had earned a stream of fellowships and was on the path to tenure at one of Boston’s preeminent universities. But James had a problem: he dreaded speaking in public. Academic conferences terrified him, so he avoided them whenever possible. He rarely interacted with colleagues. As a result, his ideas didn’t circulate and his career stalled.
In frustration, James sought help from a psychiatrist, who diagnosed him with a mental disorder known as “social phobia” and prescribed a well-known antidepressant effective in the treatment of extreme inhibition. The medication alleviated his severe anxiety and enabled him to do the things he previously couldn’t do. His work gained public recognition, and he has subsequently risen to the top of his profession.
In recent years, James’s story has become increasingly common. Using an ever-expanding arsenal of neurochemical drugs, physicians now treat variants of mood and temperament that previous generations viewed as an inescapable part of life. In an earlier era, James’s fears might have forced him to change professions. Today, the exceptionally shy and the overly anxious, the hyperactive and the chronically unhappy can seek relief from their suffering though medical intervention. And the parameters of what constitutes a “mental disorder” have swelled. An estimated 22 million Americans currently take psychotropic medications—most for relatively mild conditions.
This widespread embrace of biological remedies to life’s problems raises troubling questions for psychiatry. Paradoxically, even though psychopharmaceutical sales have soared in the United States during the past 20 years, only half of those with severe disorders receive adequate treatment. Clinicians and researchers disagree over what the priorities of the field should be and whom they should count as mentally ill. Are we over-treating the normal at the expense of the truly disturbed? Can we adequately distinguish illness from idiosyncrasy, disease from discontent? And are we allowing pharmaceutical companies and insurers to define the boundary between illness and health?
The Slippery Slope of Diagnosis
Illustration by Ken Orvidas
A recent survey estimated that nearly half of all Americans will suffer a mental illness during their lifetimes. Harvard Medical School professor of health policy Ronald Kessler headed the two-year study, which polled 9,000 adults across the country, varying in age, education level, and marital status. Researchers conducted home-based, face-to-face interviews, using the World Health Organization’s (WHO) diagnostic mental-health survey. They found that 29 percent of people experience some form of anxiety disorder, closely followed by impulse-control disorders (25 percent) and mood disorders (20 percent). Most cases begin in adolescence or early adulthood, and often, more than one disorder will strike simultaneously.
The study has sparked heated controversy. Critics argue that the numbers reflect a gross inflation of the meaning of “disease” that blurs the line between “real” disorders and normal forms of emotional and mental suffering. “By medicalizing ordinary unhappiness,” says professor of psychiatry and medical anthropology Arthur Kleinman, who is also Rabb professor of anthropology, “we risk doing a disservice to those people who have severe mental illnesses.” Kleinman fears that including mild forms of anxiety and depression under an ever-widening umbrella of mental disorders will divert attention and resources from diseases like schizophrenia and major depression, which remain undertreated and stigmatized across much of the world (see “A Deadly Emotional Disease,” page 91). In his view, “We may turn off the public, who are a huge source of support for mental-health research, by telling them that half of them are mad.”
Kessler dismisses Kleinman’s criticism as the “false enthusiasm of the noncombatant”—by which he means that if you haven’t worked directly with people who suffer from so-called mild disorders, it’s easy to write them off as ordinary. (Kleinman has been involved in developing global mental-health policy and programs with WHO; much of his research has focused on the cross-cultural study of mental illnesses such as schizophrenia and depression.) “Social phobia can be extremely debilitating,” Kessler explains. “There are people who have absolutely no friends, no support system. Their lives are incredibly small and solitary. Many say they would rather have cancer.” He points out that common mood and anxiety disorders also exact an enormous social burden in terms of days missed from work, cost to employers, and, in the worst cases, suicide. By contrast, he says, schizophrenia affects just 1 percent of the population.
At the heart of a debate over epidemiological statistics are deep misgivings about the way psychiatry defines and measures mental illness. Despite major advances in the treatment of psychiatric symptoms in recent years, there are still no definitive clinical tests to determine whether someone has a given disorder or not. “We have no equivalent of a blood-pressure cuff or blood test or brain scan that is diagnostic,” says University provost Steven E. Hyman, professor of neurobiology and the former director of the National Institute of Mental Health. The genetics of mental illness are also “fiendishly complex,” he says; although there is evidence that many conditions run in families, science has yet to identify the particular genes responsible for any disorder.
Without clear biological markers, researchers and clinicians must rely on interviews to assess the occurrence and severity of mental disorders. Interview questions follow criteria from the Diagnostic and Statistical Manual of Mental Disorders (DSM)—a 1,000-page volume covering the gamut of human affect and behavior, from mood and personality to sexuality and addiction. Researchers have arrived at the syndromes listed in the DSM by tracking symptoms and symptom clusters, with particular attention to duration, age of onset, family prevalence, gender distribution, and response to treatment. Now in its revised fourth edition, the DSM has provided the field with a common language for identifying and discussing the enormous range of mental-health problems, yet it remains more a proximate description than a verifiable picture of reality.
“The DSM has given us reliability, meaning that—armed with the DSM criteria—two different observers should arrive at the same diagnosis in the same person,” says Hyman. “But it has not given us validity.” That is, one can’t be sure that the various named disorders identify distinct syndromes in the brain. In the case of personality disorders, for instance, “If you get one diagnosis, you’re likely to get two or three or five,” Hyman points out. Similarly, people with depression often suffer from anxiety as well. “The proliferation of disorders in a single person,” he says, “suggests there is something wrong with the number of discrete diagnoses.”
This uncertainty at the core of psychiatry creates a slippery diagnostic slope. Severe illnesses, such as schizophrenia and major depression, tend to present relatively clear signs (delusions, hallucinations, catatonia, psychomotor problems). But milder disorders of mood and anxiety can share symptoms with ordinary reactions to life events. Kleinman contends that the high mental-illness rates recorded by Kessler reflect an over-reliance on a survey methodology that ignores the limitations of the science. “Lacking any laboratory tests,” he says, “there’s a tendency to let everything hang on questionnaires that researchers can even administer by telephone, using superficial questions and simple terms that can confuse the borderline between the normal and the abnormal.”
Occurrence of Eight Most Common Mental Disorders (excluding substance-abuse disorders) | |
Major depressive disorder | 16.6 % |
Specific phobia | 12.5 % |
Social phobia | 12.1 % |
Conduct disorder | 9.5 % |
Oppositional-defiant disorder | 8.5 % |
Attention deficit/hyperactivity disorder | 8.1 % |
Generalized anxiety disorder | 5.7 % |
Intermittent explosive disorder | 5.2 % |
Survey sample: 9,282 adults, 18 to 75 years of age | |
Lifetime prevalence, from Ronald Kessler’s National Co-Morbidity Survey Replication, 2005 | |
Kleinman believes the weaknesses of psychiatric measurement are detrimental not only to the severely mentally ill, but also to the rest of us. The expansion of illness categories, he says, risks turning the most profound human experiences into medical problems. Grief over the loss of a loved one, or sadness in the face of death, for example, can look like depressive disorder, according to a checklist of DSM criteria. Doctors now routinely prescribe antidepressants to terminal patients on cancer wards and to bereaved family members whose grief symptoms persist beyond the DSM’s “normal” two-month period. By making the emotions that accompany loss and dying into disease, Kleinman says, we are in danger as a society of flattening out our moral life. “The intent may be: why should anyone have to feel any degree of suffering?” he says. “And the result may be: if you make it difficult for people to engage suffering, you may actually change the nature of the world we live in.” (He takes up these issues in a new book, What Really Matters: Living a Moral Life amidst Uncertainty and Danger.)
Kessler and others involved in the measurement of mental disorders argue, on the other hand, that the advantage of catching cases early far outweighs the danger of over-counting. They compare mental illness to other medical markers, like blood pressure and cholesterol, for which definitions of disease are relative rather than absolute. As associate professor of psychiatry James Hudson, the director of the psychiatric epidemiology research program at McLean Hospital, points out, “The definition of ‘high’ blood pressure changes about every five years. Researchers come to an agreed-upon number by seeing that above a certain pressure there are more likely to be negative outcomes in terms of poor health. The blood pressure itself is not a disease, but a marker of risk.” Depression and anxiety, Kessler says, similarly exist along a gradient: “The question is where on the spectrum a person starts tipping toward bad outcomes, such as isolation, job loss, or suicide.”
Given the subjective nature of psychiatric diagnosis, determining the tipping point for mental illness is trickier than for purely physical conditions. Here the influence of drugs has been decisive. The introduction of relatively safe and effective psychotropic drugs like fluoxetine (Prozac, manufactured by Lilly), which can treat a range of psychiatric symptoms with few side effects, has increased the rate of diagnosis for many of the milder mood and anxiety disorders. There is no such thing as real depression, Kessler says. The question is: are the symptoms clinically significant enough to treat? The answer depends on whether we have a clinically effective way of treating it.
Chemical remedies thus play a role in measuring and defining mental disorders. But skeptics warn that if clinicians’ mere ability to treat symptoms identifies something as illness, disease categories will continue to expand while doctors’ understanding of what they are treating will remain imprecise.
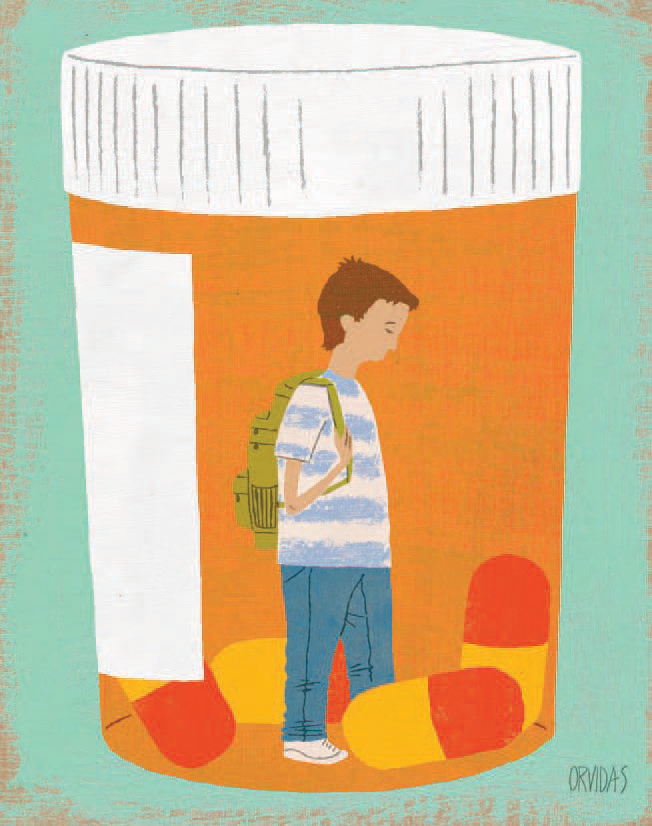
Illustration by Ken Orvidas
Diseases du Jour?
These concerns have flared over the diagnosis of “social phobia” (also called “social anxiety disorder”), which in just two decades has gone from “rare” (as listed in the DSM-III) to “common” (according to Kessler’s national statistics). Critics believe that aggressive marketing by GlaxoSmithKline of its drug Paxil, an antidepressant effective in the treatment of shyness, has inflated the category. “Ten years ago, psychiatrists might see two or three cases of social phobia a year,” says Joseph Glenmullen, a clinical instructor in psychiatry and a staff psychiatrist at Harvard Health Services. “These were people who were afraid to go to a movie because they were afraid of drawing attention to themselves if they had to get up to use the bathroom. They were terrified they wouldn’t be able to get to the exit quickly enough.” Since then, the condition has become ubiquitous. In 2001, the National Institute of Mental Health estimated that some five million American adults (nearly 4 percent of the adult population) suffer from social anxiety disorder. Diagnostic questions from national surveys identify symptoms that could apply to nearly anyone, such as: “Did you ever feel shy, afraid, or uncomfortable…meeting new people? Speaking up at a meeting? Giving a talk in front of an audience? Being in a dating situation?”
Clinicians who specialize in social anxiety emphasize the damage the disorder can inflict on lives. Associate professor of psychiatry Mark Pollack, director of the Center for Anxiety and Traumatic Stress Disorders at Massachusetts General Hospital, says that one of the hallmarks of social phobia is that people will make decisions about their careers based on their fears of interacting with new people or standing upin front of an audience. Many sufferers have struggled with anxiety since early adolescence, he says, but never thought they could do anything to change it. “Maybe they start having problems raising their hand in class. And if it makes them anxious to get up in front of a group, it’s going to affect how they interview for college and it could even affect their willingness to go to college,” he says. “So it can have an impact on their educational attainment and their ability to make a living.”
Critics question whether intense shyness and fear of public speaking are signs of pathology or simply a disadvantageous personality trait. Many occupations today require public speaking, but “this does not make natural fear of such activities a disorder,” a commentator in the Canadian Journal of Psychiatry points out, “any more than the fact that few people are smart enough to be physicists, tall enough to be basketball players, or beautiful enough to be models makes the rest of us disordered.”
The groundbreaking work of developmental psychologist Jerome Kagan, Starch professor of psychology emeritus, has shown that humans inherit certain temperamental dispositions. Kagan demonstrated that 15 percent of infants are “high reactive”—that is, electroencephalograph tests show activation of the amygdala, indicating distress, when these babies encounter unfamiliar people or things. Depending on environmental conditions, some of these innately tense children, Kagan argues, will grow into socially anxious adults, while others may overcome fear of strangers but retain anxiety to other stimuli.
Kagan’s work on innate temperament has bolstered research into the organic basis of social phobia and other anxiety conditions. But in recent years, Kagan himself has questioned a diagnostic approach that, he believes, formulaically equates impairing symptoms with a biological condition warranting medical treatment. “To say that 28 percent of Americans have anxiety disorders,” he says, referring to Kessler’s recent study, “assumes that being anxious is like having cancer. But anxiety is part of being human.” There are many ways to develop the symptoms of what’s called social phobia, he explains. “You could have a scar on your face that makes you extremely self-conscious, or you could live in a place where you feel that you’re less educated than everyone else around you. And then there’s a temperamental bias.” Kagan believes psychiatry needs to unpack the different routes leading to anxiety and other mental disorders in order to develop a wider range of appropriate treatments. But at the moment, he says, “Psychiatrists are smug. Their attitude is: ‘We have these drugs, so why should we change?’”
A similar controversy has erupted over the diagnosis of attention deficit hyperactivity disorder (ADHD). Leon Eisenberg, Presley professor of social medicine emeritus, was among the first pediatric psychiatrists to conduct research into the biomedical treatment of ADHD in children. He recalls how the introduction, in the early 1960s, of Dexedrine to treat overactive and distracted kids brought a welcome sense of efficacy to doctors and great relief to parents, who could finally attribute their childs problem to an organic disorder, rather than to their own failings. Biological diagnosis also allowed for a more economical approach to treatment, he says: Give a pill and youre done. But Eisenberg now believes that the short-term studies he conducted on Dexedrine were misleading. We tracked kids for 12 weeks, and the results were clear and made sense: if you reduce distractibility, learning should improve. Yet subsequent long-term studies have shown that if you dont incorporate a psychosocial approach, with a focus on family and learning environment, the gains dont hold.
Unfortunately, Eisenberg says, exuberance over ready solutions to complex conditions has overshadowed the need for careful diagnosis and led to over-prescribing of drugs. Soaring prescription rates for Ritalin and newer stimulants, especially among boys in achievement-focused middle-class communities, suggest a disease category run amok. “The trouble is that the drugs work across the board,” Eisenberg points out. “Dexedrine makes not only hyperkinetic kids mellower and less distractable, but normal kids as well.”
Doctors wrote some 29 million prescriptions for Ritalin and similar drugs last year in the United States—nearly 80 percent of them for children. But in recent years, treatment for ADHD has also expanded among adults. Women are just as likely as men to take the drugs. College students around the country use stimulant medications for help when studying for exams. Despite growing evidence that these drugs may increase the risk of heart arrhythmias and stroke in some patients, the use of ADHD medications grew faster between 2000 and 2004 than the use of any other class of drugs except treatments for rheumatoid arthritis.
Claims of over-diagnosis provoke considerable rancor on the front lines of ADHD treatment, where professor of psychiatry Joseph Biederman, chief of pediatric psychopharmacology at Massachusetts General Hospital, currently reigns. The most cited scientist on the subject of ADD (attention deficit disorder) and ADHD during the past decade, Biederman cites evidence from genetic and molecular imaging studies, as well as from epidemiological statistics from across the world, that in his view confirm ADHD as “a universal biological condition” that can extend into adulthood with potentially devastating consequences. Far from being overtreated, he says, “at least half the kids with the diagnosis are not treated at all,” largely because of fears of using medications in children. There’s a seven-year average gap from the time of the onset of symptoms to the onset of treatment, he says. “If this were a cavity,” he asks, “would you dare leave it untreated this long?”

Illustration by Ken Orvidas
Chemicals Preferred
Statistics suggest that there are gross inconsistencies in the delivery and quality of psychiatric care. According to Kessler’s study, close to 60 percent of people with serious disorders received no treatment between 2000 and 2003, but nearly half of the people who did receive treatment “did not meet diagnostic criteria for a mental disorder.” In other words, the mildest cases (and non-cases) may be receiving the bulk of the “cures,” while many of the severely ill are falling through the cracks.
Powerful economic forces contribute to this paradox and are exacerbating psychiatry’s disputes. Increasingly, it is not specialists such as Pollack and Biederman who do much of the diagnosing and prescribing, but rather family-medicine doctors who often lack the knowledge or opportunities to act in patients’ best interests.
Consider the case of Dora, described by Joseph Glenmullen in his book Prozac Backlash. When Dora, a schoolteacher, retired, she expected to enjoy her new freedom, especially the chance to spend time with her grandchildren. But after six months, she began to feel down. She missed her job and the sense of purpose it had provided. Her primary-care doctor told her that she was suffering from depression and, after a 20-minute consultation, gave her a year’s prescription for Prozac. He did not schedule a follow-up appointment. The medicine relieved Dora’s immediate symptoms of depression, but also left her feeling fatigued. When the year was up, she called her doctor’s office, wondering whether she should continue the treatment. The secretary told her to leave a voicemail message letting him know she was running out of medication. To Dora’s dismay, the doctor simply called in a renewal of her prescription without seeing her.
Dora eventually sought an opinion from Glenmullen. He learned that she had witnessed the murder of her parents by Nazi soldiers as a child in Budapest, and had then been shipped to Auschwitz with her grandmother, who was sent straight to the gas chambers. After the war, Dora moved to the United States, married, raised a family, and taught for 30 years. “All her life, she worked hard to survive and to put the horrible Holocaust memories out of her mind,” Glenmullen explains. But she had more time on her hands after retiring, and the painful memories returned.
During a six-month course of psychotherapy, Dora was able to address her long-suppressed feelings. She eased off the drugs and her depression did not return. Talking about the secrets from her past was a relief—and so was overcoming dependence on medication. “How could [Dora’s] HMO have failed to inquire even minimally into her psychological state and life history?” Glenmullen writes. “Are Holocaust memories really a ‘disease,’ a ‘biochemical imbalance’ that should be ‘corrected’ with a pill?”
In recent years, to reduce costs, the managed-care system has encouraged primary-care doctors with no psychiatric training to treat the more common mental-health problems. Physicians follow treatment “protocols”—formulas dictating when to prescribe medications—based on simple symptom checklists. Under pressure to keep expenses down and meet service quotas, doctors have little time to discuss a patient’s history or current circumstances. Glenmullen points out in Prozac Backlash that the introduction of the SSRI (selective serotonin reuptake inhibitor) antidepressants such as Prozac, Paxil, and Zoloft, with their one-size-fits-all-patients ease of use and broad applicability for dozens of conditions, has facilitated the outsourcing of mental-health care: [M]anaged-care insurers, he writes, [have] pressed primary-care doctors to limit the treatment of depression and psychiatric conditions to drugs with no regard whatever for the long-term consequences for patients.
Ronald Kessler’s findings suggest that these policies undermine the quality of care patients receive. The number of people seeking mental-health treatment from general practitioners has increased by 150 percent in the past 10 years. In many cases, Kessler points out, the physician didn’t complete the necessary clinical assessment, didn’t prescribe the appropriate therapy, or failed to provide ongoing monitoring. Based on these criteria, he asserts, only 12.7 percent of patients receiving treatment in this sector obtained “an acceptable standard of care.”
Insurance coverage in this country has a long history of discrimination against mental-health services, which do not have as clear a record of proven “cures” as the rest of medicine. During the past few decades, as prescription-drug coverage has expanded, insurers have covered psychotropic drugs at parity with other medical treatments, but to minimize costs, they have separated the rest of mental-health care from general medical benefits through a system of “carve-outs”—contract arrangements with specialty vendors, known as managed behavioral healthcare groups (MBHCs), which are ruthlessly cost-efficient.
A typical MBHC carve-out manages inpatient, outpatient, residential, and intensive outpatient services, but does not cover medications. As professor of health economics Richard Frank explains in a recent article in the Milbank Quarterly: “Prescription drugs are ‘free inputs’ to the specialty mental-health delivery system, and carve-out vendors have a strong economic incentive to substitute drug treatments for other mental-health services when possible. They do this by making it easier for patients to obtain referrals for medication management and psychopharmacology than referrals for psychotherapy.” According to Frank, carve-out arrangements—under both private insurance plans and Medicaid—have increased overall prescription rates for psychotropic drugs.
At the same time, pharmaceutical companies have worked hard to promote their products to doctors and to the public. Drug marketers have traditionally focused their efforts on physicians, who have long been the key decision-makers in the choice of a prescription medication for a patient. Sales representatives make visits to doctor’s offices to describe their products in a practice known as “detailing.” They often provide lunch as an incentive, and they always leave plenty of free samples behind. The companies also sponsor professional-education events for physicians—often in enticing locales like Hawaii—in an effort to build brand loyalty.
Medical journals offer an additional venue for drug marketing, because pharmaceutical companies fund much scientific research today. Although study authors must include a conflict-of-interest statement at the end of each published article, commercial sponsorship influences the production of scientific evidence in a pervasive way. “Even when conflicts of interest are disclosed and data are clear,” says senior lecturer in the department of social medicine Marcia Angell, a vocal critic of the pharmaceutical industry, author of The Truth about the Drug Companies and a former editor of the New England Journal of Medicine, “there can be manipulation of data, the study design can load the dice, and how the article is written can sway the reader.” As Leon Eisenberg points out, “If you’re getting consulting fees or lab financing from a company, it’s hard to bite the hand that feeds you by publishing negative results for their product.”
For antidepressant drugs, where non-psychiatrists write an estimated 40 percent of prescriptions, pharmaceutical marketing has had an unavoidable impact on physician practice. “Primary-care doctors are getting their information and education on depression and treatment from the pharmaceutical companies,” says Meredith Rosenthal, assistant professor of health and social policy in the Harvard School of Public Health. “This is not unbiased information.” A Harvard-educated physician in a Manhattan practice confirms this point: “There’s no question,” she confides, “that having the samples right there in the cabinet influences which medication I’m going to give to a patient.”
In recent years, the aggressive advertising of drugs directly to consumers has also boosted demand for psychotropic medications and influenced physician behavior. The amount the pharmaceutical industry spent on television and print advertisements aimed at the public grew exponentially during the 1990s, particularly after the Food and Drug Administration released guidelines for the practice in 1997. (In 2004, drug companies spent $193 million on direct-to-consumer advertising for antidepressant medications, up from $85 million in 1999.) A Prevention Magazine survey in 2002 showed that 90 percent of the public have seen prescription-drug advertisements, and, according to a 2004 study published in the journal Medical Care, exposure to ads increases the likelihood of using a psychotropic medication to treat depression.
Researchers suggest that television commercials, such as those for the antidepressants Zoloft and Paxil, have had some positive effects on treatment by reducing the stigma associated with mental-health problems. “The good news is that many people now come in [for treatment] who have serious problems, who otherwise might not,” says Richard Frank. “Considering that depression is generally viewed as under-treated, this is the upside.”
But the ads also create demand in the absence of real need. A 2005 study that used professional actors posing as patients found that when people with depression make a medication suggestion to a doctor, they increase their chances of getting appropriate treatment. Yet when people without clear criteria for depression request a brand-name medication, they, too, are more likely to get a drug. “The thing that’s disturbing,” says Frank about the study, “is that, to a large extent, we kind of count on the doctor to help the patient separate the wheat from the chaff. Yet it seems [doctors] are prone to the same advertising signals [as] the rest of us.”
It’s clear that aggressive pharmaceutical marketing in combination with cost-cutting care has led to increased reliance on psychotropic drugs to the exclusion of other forms of treatment. Although many mental disorders clearly warrant medications, there are plenty of cases like Dora’s in which nonmedical therapies are effective and probably more cost-efficient over the long term. Jack Gorman, president and psychiatrist-in-chief at McLean Hospital and lecturer on psychiatry at Harvard Medical School, believes that valuable psychosocial treatments are being underutilized, often to patients’ detriment. He points in particular to cognitive and behavioral therapies that are “evidence-based” and superior to medication in many instances for treating anxiety and depressive disorders. (Behavioral therapy, for example, works on the principle that, if people are exposed to the situations they fear, they will eventually become desensitized and thus able to do things they couldn’t do before.) “Unfortunately, the people developing these therapies don’t have the huge marketing budgets that the drug companies have,” Gorman says, “and managed-care companies just assume it’s cheaper to give everybody a medication.”
Quick, Material Solutions
Drug companies and health insurers are not the only ones responsible for our growing dependence on psychopharmaceuticals. “We’re all unindicted co-conspirators,” as Monrad professor of the social sciences Charles Rosenberg, an historian of science, puts it.
Americans are living in a cultural moment when the idea of a quick, material solution to psychic and emotional pain is extremely appealing. “As a society,” Rosenberg says, “we’ve never been more infatuated with visions of molecular and neurochemical—ultimately genetic—truth.” If our children are unmanageable, we are thankful for a diagnosis that shifts the blame from us to nature and offers the prospect of a tangible cure. If our fears of underperforming in our jobs or our marriages make us less productive, the lure of medication may be hard to resist. (If the guy in the next cubicle is on it, shouldn’t I be?) The Harvard-educated physician in New York City reports that requests for antidepressants have increased most recently among her Wall Street patients. “They’re stressed about work, about their mortgages, about their kids’ school problems,” she says. “They want to stay competitive.” Psychotherapy takes time and may not work—and who can afford to fall behind?
Psychiatry’s crisis is not simply a problem of diagnostic precision or of misplaced economic priorities; it is also a moral predicament that reflects our times. How much of ourselves are we willing to give over to forces of scientific and technical control? Depression and anxiety are complex conditions; they don’t look the same in any two people. Although we may ultimately find the genes responsible for making some of us more anxious and melancholy than others, psychiatry will never fit neatly into the biological sciences. Treatment will still have to take account of experience, the social environment, and human subjectivity. At some point, we will have to look beyond immediate symptoms if we hope to address the reasons for so much anxiety and dysphoria in our society. Jerome Kagan offers a useful analogy:
There’s a place in a large city with very bad drinking water, and kids are always getting sick with dysentery. So you keep treating the dysentery, but meanwhile it would be much better to clean up the drinking water….The drugs work on the dysentery for about 48 hours, but you’re not treating the problem. And the problem is not genetic.
Ashley Pettus ’87 is a freelance writer living in Cambridge.