Ever since the earliest reports of a pneumonia-like illness spreading within Hubei province in China, the resemblance to the SARS outbreak of 2002-2003 has been uncanny: probable origins in the wild-animal markets of China; an illness that in some people resembles the common cold or a flu, but in others leads to pneumonia-like symptoms that can cause respiratory failure; community transmission that often occurs undetected; super-spreader events; and reported vertical transmission in high-rises or other living spaces where the waste systems are improperly engineered or drain catch-basins are dry, allowing aerosolized particles to pass from one floor of a building to another (see “The SARS Scare” for an in-depth description of the epidemiology and virology of the SARS outbreak of 2002-2003 and the four independent zoonotic transmissions of 2003-2004).
UPDATED 3-04-2020 at 12:57 p.m. See below.
At first, this latest outbreak was referred to as a novel coronavirus, then in the media as COVID-19 (formally, the name for the disease in an infected person who has become sick, a distinction analogous to that between a person who is HIV positive and one who has developed AIDS). Now that the virus has been characterized and its relationship to SARS firmly established, its designation is SARS-CoV-2—severe acute respiratory syndrome coronavirus 2.
Will public-health measures be sufficient to contain its spread? How infectious is it? What is the incubation period? Is this a pandemic? What role does the immune-system response play in the progression of the disease? Which populations are most at risk? Can scientists develop a vaccine, and how quickly? These are some of the questions that scientists worldwide are asking, and that a collaboration among Harvard University and Chinese researchers will address as part of a $115-million research initiative funded by China Evergrande Group, which has previously supported University green-buildings research at the Graduate School of Design, research on immunologic diseases, and work in mathematics. (See below for the University press release describing the initiative.)
Harvard Magazine spoke with some of the researchers involved in fighting the first SARS outbreak, and those who will be collaborating with Chinese colleagues, in what is already a worldwide effort to control SARS-CoV-2.
The Virus
Michael Farzan ’82, Ph.D. ’97, who in 2002 was an assistant professor of microbiology and molecular genetics at Harvard Medical School (HMS) studying the mechanism that viruses use to enter cells, was the first person to identify the receptor that SARS used to bind and infect human cells. “SARS-CoV-2 is a close cousin to SARS, and uses the same human receptor, ACE2,” reports Farzan, who is now co-chair of the department of immunology and microbiology at Scripps Research. The ACE2 receptor is expressed almost exclusively in the lungs, gastrointestinal tract, and the kidneys, which explains why the disease is so effectively transmitted via both the respiratory and fecal-oral routes.
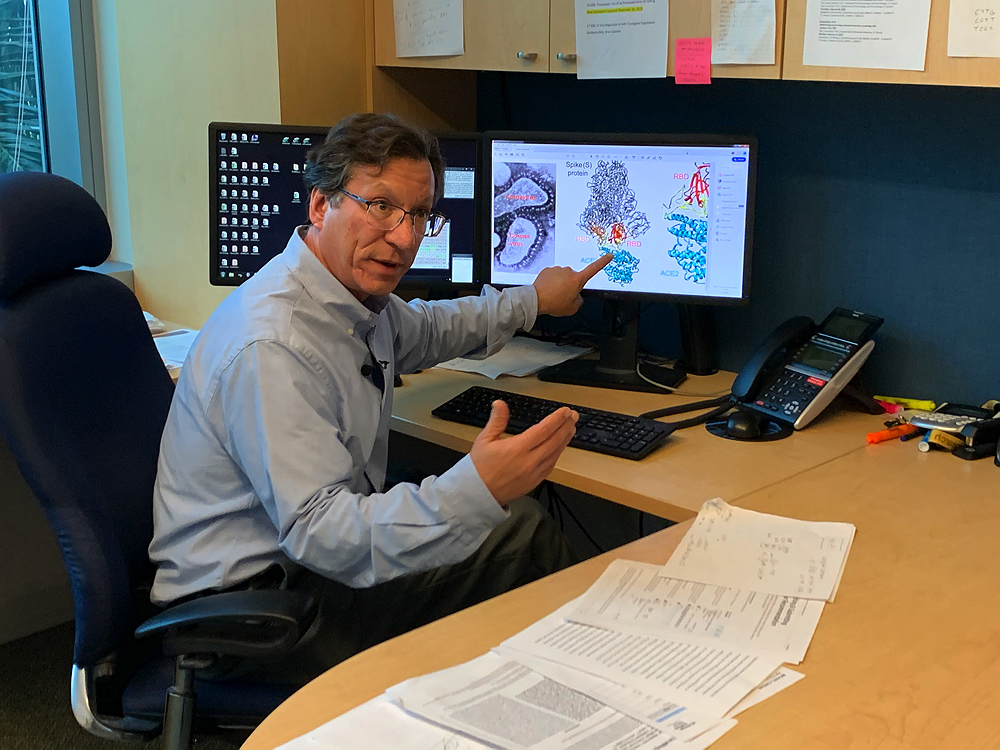
Michael Farzan ’82, Ph.D. ’97, pointing to an ACE2 receptor (cyan) binding to a SARS-CoV-2 spike protein (gray/red)
Photograph courtesy of Michael Farzan
But there are “subtle differences” in the new virus behind the current outbreak, he explained in an interview. The virus’s receptor binding domain—the part that attaches to the human receptor—“has undergone a lot of what we call positive selection, meaning there has been a good deal of evolutionary pressure on that region from natural antibodies, probably in bats” or some other animal host that is a reservoir for this disease. “So while the virus retains its ability to bind ACE2,” Farzan explains, “it no longer binds the same antibodies.” That is unfortunate, because as the first SARS epidemic wound down, HMS professor of medicine Wayne Marasco had identified a single antibody—from what was then a 27-billion antibody library—that blocked the virus from entering human cells. (Marasco is actively testing new antibodies, hoping to find one that will have the same effect on SARS-CoV-2. For more on Marasco’s work, see below.) Still, “we are not starting from square one,” says Farzan.
“In animal studies, Remdesivir” [a new and experimental antiviral drug] has seemed to work against SARS-like viruses, he says. “Its effectiveness will probably hinge on getting it early enough,” in the same way that the antiviral drug Tamiflu® is most effective against the seasonal flu when given to patients early in the course of infection.
And there is a reasonable hope that a vaccine can be developed, Farzan adds, because the part of the virus that binds the human receptor “is exposed and accessible,” making it vulnerable to the immune system’s antibodies. In addition, the viral genome is relatively stable. That means SARS CoV-2 won’t evolve much over the course of an epidemic, so a vaccine that is relatively protective at the beginning of an epidemic will remain effective until its end.
Another reason for optimism—despite the long road to deploying any vaccine in humans—is that the science that allows researchers to understand the virus’s structure, life cycle, and vulnerabilities is progressing far more rapidly today than during the first SARS outbreak 17 years ago. So, too, is the understanding of the human immune response to the virus, and of the most effective public-health strategies based on the epidemiology of the disease.
The Epidemiology
When epidemiologists assess the severity of an epidemic, they want to know how effectively the disease can propagate in a population. The first measure they attempt to calculate is the reproductive number (R0)—the number of people that an infected individual will in turn infect in an unexposed population, in the absence of interventions. When the reproductive number is greater than 1 (meaning each infected person in turn infects more than one other person), more and more people become infected, and an epidemic begins. Public-health interventions are therefore designed to lower the rate of transmission below 1, which eventually causes the epidemic to wind down. The second number epidemiologists focus on is the serial interval—how long it takes one infected person at a particular stage of the disease to infect another person to the point of the same stage of the disease. The serial interval thus suggests how rapidly the disease can spread, which in turn determines whether public-health officials can identify and quarantine all known contacts of an infected individual to prevent their retransmitting the disease to others.
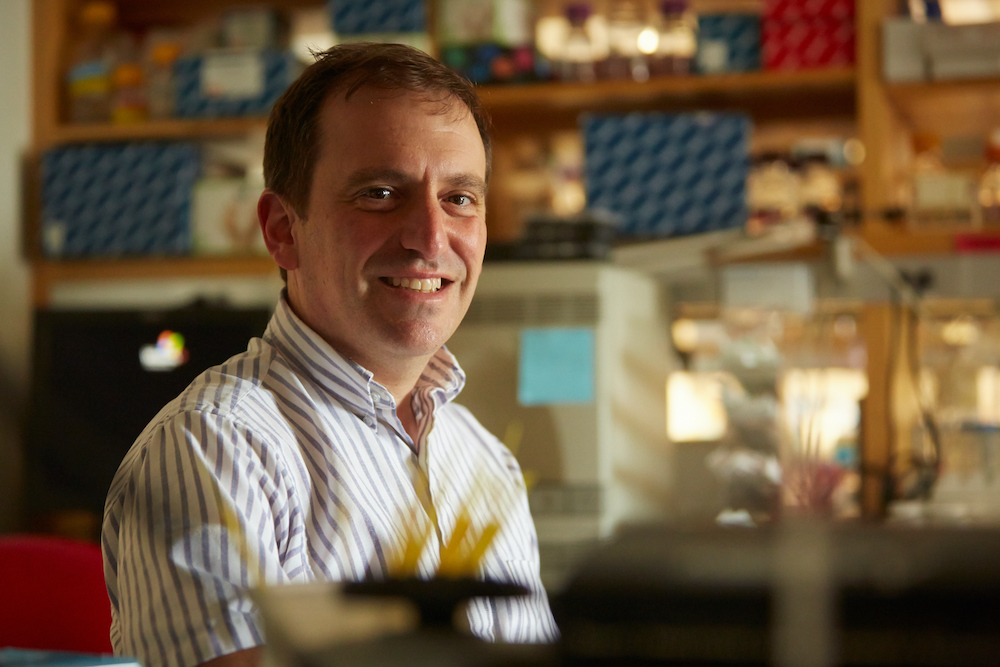
Epidemiologist Marc Lipsitch will be one of several Harvard scientists collaborating with Chinese colleagues to fight SARS-CoV-2
Photograph by Kent Dayton
Marc Lipsitch, a professor of epidemiology at the Harvard Chan School of Public Health (HSPH), and director of the school’s Center for Communicable Disease Dynamics, helped lead one of the two teams that first calculated the reproductive number of SARS in the 2002-2003 outbreak. SARS had an R0 of 3, he recalls: each case led to three others. In that outbreak, about 10 percent of those who became sick died. The good news is that SARS CoV-2 appears to have a much lower R0 than SARS, ranging from the high ones to low twos, and only 1 percent to 2 percent of those who become sick have died. [Subsequent research suggests that the R0 of SARS CoV-2 could be much higher than this] On the other hand, the serial interval—still being worked out—appears to be shorter, meaning the new virus has the potential to spread faster.
In the current epidemic, Lipsitch notes a further concern: the fact that the incubation-period distribution and the serial-interval distribution are almost identical. That’s a mathematical way of saying that people can start transmitting the virus even when they are pre-symptomatic, or just beginning to exhibit symptoms. That makes tracing and quarantining contacts of infected individuals—a classic, frontline public-health measure—nearly impossible.
Tracing, quarantining, and other public-health interventions, such as distancing measures (closing workplaces or asking employees to work from home, for example) proved sufficient to defeat SARS in the early 2000s. But with SARS-CoV-2, public-health measures alone may prove inadequate. Controlling this version of SARS may require antivirals, stopgap antibody therapies, and ultimately, vaccines, deployed together with robust public-health containment strategies.
Unfortunately, SARS-CoV-2 is “almost certainly already a pandemic,” Lipsitch continues: demonstrating “sustained transmission in multiple locations that will eventually reach most, if not all places on the globe. The disease appears to be transmitting pretty effectively, probably in Korea, probably in Japan, and probably in Iran.” He now estimates that 20 to 60 percent [figures updated 03-04-2020 at 12:57 p.m.] of the adult global population will eventually become infected.
That said, “Infected is different from sick,” he is careful to point out. “Only some of those people who become infected will become sick.” As noted above, only about 1 percent to 2 percent of those who have become sick thus far have died, he says. But the number of people who are infected may be far greater than the number of those who are sick. “In a way,” he says, “that’s really good news. Because if every person who had the disease was also sick, then that would imply gigantic numbers” of deaths from the disease.
The Collaboration
“I'm very gratified,” Lipsitch continues, “to see that both China and Harvard recognize the complementarity between public health and epidemiology on the one hand, and countermeasure-development on the other hand. We can help target the use of scarce countermeasures [such as antivirals or experimental vaccines] better if we understand the epidemiology; and we will understand the epidemiology better if we have good diagnostics, which is one of the things being developed in this proposal. These approaches are truly complementary.”
In the short term, Lipsitch—who has sought to expand the modeling activities of the Center for Communicable Disease Dynamics to better understand the current outbreak’s epidemiology—says, “It would be great to expand collaborations with Chinese experts.” Longer term, “I see a really good opportunity for developing new methods for analyzing data better, as we have in previous epidemics.” After the first SARS outbreak, for example, epidemiologists developed software for calculating the reproductive number of novel diseases; that software now runs on the desktop computers of epidemiologists around the world. And in 2009, during an outbreak of swine flu in Mexico, Lipsitch and others developed a method for using the incidence of the disease among a well-documented cohort of travelers who had left Mexico, to estimate the extent of the disease among a much larger and less well surveyed population of Mexican residents.
What they found then was that the estimated number of cases in Mexican residents likely exceeded the number of confirmed cases by two to three orders of magnitude. The same method is being used to assess the extent of SARS-CoV-2 in China right now—“so far without any hiccups.” In the Mexican case, Lipsitch reports, the estimates suggested that severe cases of the disease were uncommon, since the total number of cases was likely much larger than the number of confirmed cases. “So I think we have learned from each epidemic how to do more things. And in between them, you solidify that less visible, less high-profile research that builds the foundation for doing better the next time.” His group, for example, has been developing ways to make vaccine trials faster and better once a vaccine candidate exists.

David Knipe
Photograph courtesy Harvard Medical School
A vaccine is the best long-term hope for controlling a disease like SARS-CoV-2. Higgins professor of microbiology and molecular genetics David Knipe, who like Lipsitch will participate in the newly announced collaboration, works on vaccine delivery from a molecular perspective. Knipe has developed methods to use the herpes simplex virus (HSV) as a vaccine vector and has even made HSV recombinants that express the SARS spike protein—the part of the virus that binds the human ACE2 receptor. He now seeks to make HSV recombinants that express the new coronavirus spike protein as a potential vaccine vector.
But Knipe also studies the initial host-cell response to virus infection, which is sometimes called the innate immune response. And he has used HSV vectors that expressed the first SARS spike protein to study how it activates innate immune signaling. That is important because in SARS 1, initial symptoms lasted about a week, but it was the second phase—characterized by a massive immune-system response that began to damage lung tissue—that led to low levels of oxygen saturation in the blood, and even death. “The inflammation in the lungs is basically a cytokine storm,” an overwhelming and destructive immune response “that’s the result of innate signaling,” Knipe explains. “So we’re going to look at that with the new coronavirus spike protein, as well. This could help to determine the actual mechanism of inflammation, and then we can screen for inhibitors of that that might be able to alleviate the disease symptoms.”
The idea, he says, is to stop the inflammatory response now killing people in the respiratory phase of the disease by targeting “the specific molecular interaction between the virus and the host cell.” This, he explains, aligns with one of the principal initial goals of the collaboration, which is to support research both in China and at Harvard to address the acute medical needs of infected individuals during the current crisis.
Another form of frontline defense against the virus is antibody therapy. In an epidemic, this type of therapy is usually administered as a prophylaxis to first responders at high risk of infection, or as treatment to patients who are already sick or to people who might be harmed by a vaccine, such as pregnant women, the elderly, or those with co-morbidities. Wayne Marasco, an HMS professor with a lab at the Dana Farber Cancer Institute, was the first to develop antibody therapies against SARS and MERS, a related coronavirus, in 2014. What he learned in those outbreaks was that using only a single antibody to bind the virus’s receptor binding domain—the part of the virus that attaches to the human receptor—is not enough to prevent “escape” through mutations that neutralize the therapy. “You have to use combinations of antibodies to block the escape pathways,” he explains. But the combinations “have to be carefully designed” to avoid the risk that the virus will evolve a “gain of function”—or “the virus coming out of the patient is more pathogenic than the virus you started to treat.”
During the MERS outbreak, Marasco led the Defense Advanced Research Projects Agency’s 7-Day Biodefense program. DARPA “would drop an unknown pathogen off at our doorstep,” Marasco says, “and we had seven days to develop a therapeutic” that could be manufactured at scale. A second DARPA-funded project focused on reducing the cost of therapies to less than $10 a dose. “The government has made efforts to streamline that process to get the production sped up and the cost decreased,” he notes, although the efforts are “independent of regulatory approval, which has a life of its own.”
Marasco currently collaborates with an international team that can perform studies—including some that can’t be done at Harvard—thanks to ready access to a Biosafety Level 4 laboratory and to non-human primates for testing. The team is working to develop antibody therapies effective against SARS-CoV-2, but Marasco cautions that the situation “is pretty worrisome” with a disease that has a “long latency period when people show no symptoms,” and when public-health officials cannot identify source cases (as in Italy and in the single case of apparent community transmission in California reported February 26).
“The problem in getting ahead of this now,” he continues, is funding. “Government resources are generally a redistribution of funds that have previously been granted to projects such as the Ebola outbreak in West Africa, or come as administrative supplements to preexisting grants.” But “with the pace of this epidemic, a lack of resources is limiting what can get done and how quickly it can be accomplished.” Beyond the creation of therapeutics, “there are all kinds of epidemiologic considerations” that require rapid funding, from investigating modes of transmission “to field testing for infection.”
In the near term, the way to treat masses of patients, he says, is to take blood plasma from someone who has recovered and administer it to an infected person. The convalescent’s antibodies then fight the infection. “The FDA would never approve it,” he notes, but “it does work.” Ultimately, the “treatment of choice”—and the most cost-effective approach, he says, will be a vaccine.
Developing a Vaccine
“In the last days of 2019 and the first days after the New Year, we started hearing about a pneumonia-like illness in China,” says Dan Barouch, an HMS professor of medicine and of immunology known for his anti-HIV work, whose lab has developed a platform for rapid vaccine development. (During the Zika virus outbreak of 2016, for example, his group was the first to report, within a month, a vaccine protective in animal models.) “When the genome of the virus was released on Friday, January 10, we started reviewing the sequence that same evening, working through the weekend. By Monday morning, we were ready to grow it.”
Dan Barouch
Photograph courtesy Harvard Medical School
His concern about this latest outbreak was that “the rate of spread seemed to be very rapid.” In addition, the outbreak had the clinical features of an epidemic. “We reasoned that this might make it difficult to control solely by public-health measures,” he says, particularly because the virus can be “transmitted by asymptomatic individuals.” Thus, if the epidemic is still spreading toward the end of this year or early 2021, by which point a vaccine might be available, Barouch explains, such a remedy could prove essential. Historically, when viral epidemics don't self-attenuate, the best method of control is a vaccine.
Although Barouch’s Beth Israel Deaconess Medical Center lab is working on DNA and RNA vaccines, a new technology that has the potential to cut vaccine development times in half, large-scale manufacturing using so-called nucleotide vaccines is unproven. “That's why I think there needs to be multiple parallel vaccine efforts,” he emphasizes. “Ultimately, we don't know which one will be the fastest and most protective.” At the moment, he reports, “there are at least a half dozen scientifically distinct vaccine platforms that are being developed” and he believes that “vaccine development for this pathogen will probably go faster than for any other vaccine target in human history.”
“Ever since I graduated from medical school,” he points out, “there have been new emerging or re-emerging infectious disease outbreaks of global significance with a surprising and disturbing sense of regularity.” There is Ebola. There was Zika. There were SARS, MERS; the list keeps growing. “With climate change, increasing globalization, increasing travel, and population shifts, the expectation is that epidemics will not go away, and might even become more frequent.”
In this global context, Barouch emphasizes the importance of a collaborative response that involves governments, physicians, scientists in academia and in industry, and public-health officials. “It has to be a coordinated approach,” he says. “No one group can do everything. But I do think that the world has a greater sense of readiness this time to develop knowledge, drugs, and therapeutics very rapidly. The scientific knowledge that will be gained from the vaccine efforts [will] be hugely valuable in the biomedical research field, against future outbreaks, and in the development of a vaccine to terminate this epidemic.”
University provost Alan Garber, a physician himself, adds that “Global crises of such magnitude demand scientific and humanitarian collaborations across borders. Harvard and other institutions in the Boston area conduct research on diagnostics, virology, vaccine and therapeutics development, immunology, epidemiology, and many other areas….With its tremendous range of expertise and experience, our community can be an important resource for any effort to address a major global infectious disease outbreak. Our scientists and clinicians feel an obligation to be part of a promising collaboration to overcome the worldwide humanitarian crisis posed by this novel virus.”
UPDATED 3-03-2020 AT 12:10 p.m. TO INCLUDE A REPORT FROM THE MEETING WITH CHINESE COLLEAGUES
In a closed-door meeting that took place Monday, March 2, 2020, at Harvard Medical School, nearly 80 Boston-area scientists gathered to discuss with colleagues from China participating via video link how to respond to COVID-19 disease and the SARS-CoV-2 virus that causes it. This was the first meeting to take place as a result of the collaboration with scientists at the Guangzhou Institute of Respiratory Health announced on Monday, February 24. In attendance locally were experts from Harvard Medical School (HMS), the Harvard T.H. Chan School of Public Health, the HMS-affiliated hospitals, the Ragon Institute, Boston University, the Broad Institute, MIT, the Wyss Institute, as well as representatives from industry. The workshop, convened by HMS dean George Q. Daley, was a planning session to map out the process for coordinating on collaborative projects, designed to allow the participants to meet, form working groups by research area, and determine next steps.
“The collaboration harnesses the strengths of the Boston scientific and biomedical ecosystem,” the event’s organizers said in a statement, “with the critical experience of Chinese scientists, who are providing on-the-ground insight into diagnostics and care for patients on the frontlines.
“This public health crisis,” they continued, “is an opportunity to catalyze an unprecedented level of collaboration among various scientific efforts across Boston and Cambridge to address both the acute, most pressing challenges of this particular epidemic but also to establish a framework for future collaborations and create a more nimble rapid-response system for other epidemics.”
The meeting was organized according to areas of research interest, need, and opportunity including:
- Epidemiology, because studies of disease transmission, infectivity, and pathogen behavior are key to informing vaccine research and patient selection for clinical trials;
- Pathogenesis of the disease, since efficacy of vaccines and therapies are critically dependent on understanding host-pathogen interaction in key areas. To that end, researchers must use reliable animal models that mimic human disease with high fidelity to explore the host’s immune response to the virus, immunologic differences in disease across various subpopulations, including the young, adults, and older adults; and the effects of host genetics on disease course and outcome;
- Diagnostics, because the keys to clinical management of infected patients are rapid, sensitive, and highly specific tests to detect the virus, as well as the means to monitor immune responses. At the same time, detection methods that are scalable, inexpensive, and deployable at the point of care (ideally in the home) are needed to facilitate community surveillance, epidemiology, and modeling studies of disease transmission;
- Therapeutics, since both drugs and therapeutic antibodies will likely prove to be critical interventions for patients with confirmed COVID-19;
- Vaccines, since they represent the best long-term control mechanism for pandemics; and
- Clinical Management, because improving survival and recovery for the severely ill will depend on defining and sharing best-practices for clinical care based on the most up-to-date evidence.
The meeting demonstrated the need to establish a collaborative regional response capacity, not only for this outbreak, but for other future emerging infectious diseases, said the organizers. They are now working to create an organizational structure that will formalize the working groups in each of the above areas, and allow for the optimal deployment of resources including disciplinary and clinical expertise, shared “core” facilities, and funding.
The official Harvard press release follows:
Harvard University Scientists to Collaborate with Chinese Researchers
on Development of Novel Coronavirus Therapies, Improved Diagnostics
At a glance:
- Harvard University scientists will collaborate with Chinese colleagues to tackle the most pressing challenges posed by the novel coronavirus (COVID-19) disease
- Efforts aimed at elucidating the basic biology of the virus, and the resulting disease, toward new diagnostic tools, vaccine development and antiviral therapies
- The work will span basic science, translational and clinical research, epidemiology
- Collaboration is part of $115 million research initiative funded by China Evergrande Group
Since its identification in December, the novel coronavirus has quickly evolved into a global threat, taking a toll on human health, overwhelming vulnerable health care systems and destabilizing economies worldwide.
To address these challenges, Harvard University scientists will join forces with colleagues from China on a quest to develop therapies that would prevent new infections and design treatments that would alleviate existing ones.
The U.S. efforts will be spearheaded by scientists at Harvard Medical School, led by Dean George Q. Daley, working alongside colleagues from the Harvard T.H. Chan School of Public Health. Harvard Medical School will serve as the hub that brings together the expertise of basic scientists, translational investigators and clinical researchers working throughout the medical school and its affiliated hospitals and institutes, along with other regional institutions and biotech companies.
The Chinese efforts will be led by Guangzhou Institute of Respiratory Health and Zhong Nanshan, a renowned pulmonologist and epidemiologist. Zhong is also head of the Chinese 2019n-CoV Expert Taskforce and a member of the Chinese Academy of Engineering.
Through a five-year collaborative research initiative, Harvard University and Guangzhou Institute for Respiratory Health will share $115 million in research funding provided by China Evergrande Group, a Fortune Global 500 company in China.
“We are confident that the collaboration of Harvard and Guangzhou Institute of Respiratory Health will contribute valuable discoveries to this worldwide effort,” said Harvard University President Lawrence Bacow. “We are grateful for Evergrande’s leadership and generosity in facilitating this collaboration and for all the scientists and clinicians rising to the call of action in combating this emerging threat to global well-being.”
“Evergrande is honored to have the opportunity to contribute to the fight against this global public health threat,” said Hui Ka Yan, chair of the China Evergrande Group. “We thank all the scientists who responded so swiftly and enthusiastically from the Harvard community and are deeply moved by Harvard and Dr. Zhong’s team’s dedication and commitment to this humanitarian cause. We have the utmost confidence in this global collaborative team to reach impactful discoveries against the outbreak soon.”
While formal details of the collaboration are being finalized, the overarching goal of the effort is to elucidate the basic biology of the virus and its behavior and to inform disease detection and therapeutic design. The main areas of investigation will include:
- Rapid, more accurate diagnostic tests, including point-of-care testing
- Understanding the body’s immune response and host-pathogen interaction, including identification of biomarkers that can help monitor the infection course and disease progression and forecast the onset of critical illness and life-threatening complications among infected patients
- Vaccines to prevent infection
- Antiviral therapies that shorten the duration of the illness and mitigate symptoms among those infected
- Treatments for those with severe disease
“With the extraordinary scale and depth of relevant clinical and scientific capabilities in our community, Harvard Medical School is uniquely positioned to convene experts in virology, infectious disease, structural biology, pathology, vaccine development, epidemiology and public health to confront this rapidly evolving crisis,” Daley said. “Harnessing our science to tackle global health challenges is at the very heart of our mission as an institution dedicated to improving human health and well-being worldwide.”
“We are extremely encouraged by the generous gesture from Evergrande to coordinate and support the collaboration and by the overwhelmingly positive response from our Harvard colleagues,” said Zhong, who in 2003 identified another novel pathogen, the severe acute respiratory syndrome (SARS) coronavirus and described the clinical course of the infection.
“We look forward to leveraging each of our respective strengths to address the immediate and longer-term challenges and a fruitful collaboration to advance the global well-being of all people,” Zhong added.
Harvard University Provost Alan M. Garber said outbreaks of novel infections can move quickly, with a deadly effect.
“This means the response needs to be global, rapid and driven by the best science. We believe that the partnership—which includes Harvard and its affiliated institutions, other regional and U.S.-based organizations and Chinese researchers and clinicians at the front lines—offers the hope that we will soon be able to contain the threat of this novel virus,” Garber said. “The lessons we learn from this outbreak should enable us to respond to infectious disease emergencies more quickly and effectively in the future.”