Across the world, breast cancer takes a devastating toll on women. When it strikes within families, the effects can be especially far-reaching. Globally, breast cancer is by far the most common form of cancer in women, but the majority who die from the disease—58 percent—live in developing countries.
In those regions, a shortage of medical equipment and specialists hampers early detection and precise categorization of cancer type. Diagnosis can become a prolonged and costly process, taking as much as six months. Delays make the disease deadlier.
Now scientists have developed a rapid system that can accurately and inexpensively test for this all-too-common disease. Collaborating among universities and hospitals in South Korea, Singapore, and the United States, seven researchers have devised a technology named CytoPAN that accurately detects breast cancer—and identifies its subtype—in less than one hour.
Jouha Min, the lead author of the Science Translational Medicine paper that outlines CytoPAN’s effectiveness and potential uses, calls breast cancer a “special cancer because the biomarkers are well-established.” Researchers have studied it for decades, enabling them to determine the disease’s four different subtypes, says Min, who was until recently a postdoctoral fellow at the Center for Systems Biology at Massachusetts General Hospital. (The center is run by Min’s adviser and study senior author Ralph Weissleder, Thrall Family professor of radiology and professor of systems biology.) “What was missing was [testing] technology that was portable and easy for less skilled people to use,” says Min, who will become an assistant professor of chemical engineering at the University of Michigan next year.
CytoPAN could also improve health outcomes in the United States...in underdeserved areas.
The immediacy of CytoPAN’s accurate results, within minutes, is critical, because women whose specific cancer subtype is detected and treated earlier have higher survival rates than those with delayed diagnoses. “In Africa, sometimes they skip the subtype diagnosis” because of a paucity of testing resources, says Min. Instead, doctors immediately prescribe a drug effective for treating some subtypes to all patients, even though different forms of breast cancer require different treatments.
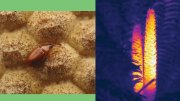
Min, Weissleder, and their colleagues developed and tested the system—which performs automated, same-day analyses of cells taken directly from patients—with funding from the National Institutes of Health. CytoPAN, an acronym derived from “portable fluorescence-based image cytometry analyzer,” takes multiple images of the cells and analyzes them using custom-designed algorithms. “For years we’ve been interested in developing new technology like this,” says assistant professor of radiology Hyungsoon Im, another co-author.
To test the new system’s effectiveness, the authors employed the technology to treat 68 patients at a hospital in Korea. The results of the tests were remarkable: CytoPAN quickly and accurately diagnosed disease 100 percent of the time with samples of as few as 50 cells. (Testing cells rather than tissue makes CytoPAN both more effective and less invasive.) The test also detects cell-based biomarkers in the samples—indicators which reveal the presence of cancer, its form, stage, and potential to respond to treatment—with more than 90 percent accuracy, a rate high enough to be useful in guiding treatment options.
The procedure is also less expensive than traditional needle-based biopsy sampling methods for cancer detection, which can cost from hundreds of dollars in low- and middle-income countries to thousands in the United States. CytoPAN machines, which cost about $3,500 apiece, require less training to operate and utilize fewer than five dollars’ worth of materials per test. Such advantages mean CytoPAN could also improve health outcomes in the United States and other developed countries, particularly in underserved areas. “Not all states have centralized hospital systems, so we could deploy this in local clinics or mobile clinics,” says Im, who notes that rural areas must sometimes send test specimens to larger, distant hospitals, further delaying results for anxious patients.
The technological breakthrough comes as the number of breast cancer cases worldwide is increasing, driven in large part by growing populations and lengthening lifespans in developing countries. In 2018, there were 18.1 million new cases and 9.6 million deaths from the disease. By 2040, the number of new cases is projected to reach 29.5 million.
Min is now working for Aikili, a startup launched as a result of the study’s findings that has received funding from Harvard and elsewhere to commercialize CytoPAN. Given the scale of the problem, even slightly increasing the number of accurate diagnoses and thereby reducing the number of deaths worldwide would be a major achievement.