A miniature device the size and shape of an aspirin tablet could provide new options for people with cancer. Developed in the lab of Pinkas Family professor of bioengineering David Mooney, the implantable vaccine, inserted under a patient’s skin, operates like a tiny factory where immune cells of one kind are transformed to train other immune cells to eradicate tumors.
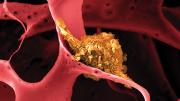
The tablet-like device emits a signal that attracts dendritic cells, the messengers of the immune system, which carry information about the pathogens and toxins they encounter to other immune cells. The dendritic cells “literally crawl inside the plastic device” to be activated by freeze-dried fragments of the patient’s own tumor, Mooney explains. Once the dendritic cells have become activated, they “home to the nearest lymph node,” where they encounter T cells that they train to recognize and destroy cancer cells. The T cells then multiply and circulate through the body, dissolving the patient’s tumor. The researchers also believe the vaccine could generate immune memory to prevent future tumor growth.
Mooney says that his bioengineering work would not be possible without groundbreaking fundamental research conducted first by immunologists who “mapped out the key cell types, key molecules, and pathways. This provided the foundation that engineers like me needed to come in and get engaged.” The device that he and his team developed through the Wyss Institute for Biologically Inspired Engineering is made of the same plastic found in biodegradable surgical sutures; it completes its activity in a few weeks and dissolves within a few months.
Immuno-oncology—which harnesses the body’s immune system to fight cancer—has progressed significantly in the last decade, offering new ways to help patients. Current cancer vaccines come in two forms, Mooney explains. One works similarly to a flu shot: a solution containing antigens (proteins from the flu virus or cancer cell) and adjuvants (which boost the body’s immune response to the antigens) is injected into the body to attack cancer cells. The other vaccine type involves nanoparticles containing the antigen and adjuvant that are placed in the body and travel to a lymph node. The new vaccine improves on these options in two ways, Mooney says. First, his team’s device works for a longer time, “so we probably end up trafficking many cells. Second, it appears that we’re able to bring in a variety of different dendritic cells to the device, and it’s likely that the combination of cells works together to generate a really effective response.”
The implantable cancer vaccine could also incorporate other cancer-fighting tools. Another project in Mooney’s lab adds chemotherapy drugs to the device, which is then implanted near a tumor, triggering cell death and enabling those tumor fragments to be passed directly to the dendritic cells for presentation to the cancer-hunting T cells. This approach showed promise in mice with triple-negative breast cancer, an especially aggressive form.
In an earlier study of the implantable vaccine, conducted in mice that would otherwise have died of metastatic melanoma, 50 percent showed complete regression of their tumors. Data on the vaccine’s effect in people is not yet available; a Phase 1 clinical trial in about 20 patients with advanced melanoma, who received the device up to four times, ended in 2019. Dana-Farber Cancer Institute oncologist F. Stephen Hodi, who led the trial, is analyzing the data and hopes to publish his findings soon. Mooney and his team, meanwhile, have conducted studies of the vaccine in animal models of different cancer types. They have seen a promising response to blood cancers such as acute myeloid leukemia (AML), and in solid tumor malignancies including breast and lung cancer, but he cautions, “It’s very different curing a mouse versus a person.”
And promising as the implantable vaccine technology may be, Mooney stresses that “there’s no magic bullet. Cancer is a lot of different diseases that we’ve lumped together, and there’s no one therapy that’s going to be the end-all across the board. We’re hoping that this vaccine will have an important role in combination with other therapies.”