A large-scale study comparing the efficacy of the Moderna and Pfizer vaccines against COVID-19 finds that Moderna’s vaccine is slightly more effective at preventing a range of outcomes, including infection, COVID-19 symptoms, hospitalization, admission to intensive care, and death. The study, published online December 1 by the New England Journal of Medicine, analyzed outcomes for about 440,000 vaccinated U.S. veterans, half of whom received Pfizer’s vaccine, and half of whom received Moderna’s, between January 4 and May 14, 2021. In these demographically and clinically matched groups, recipients of the Pfizer shot had an estimated 27 percent higher risk of documented SARS-CoV-2 infection and 70 percent higher risk of COVID-19 hospitalization during a 24-week follow-up period when the Alpha variant of SARS-CoV-2 was predominant. During a subsequent 12-week period when the Delta variant was predominant, the risk of documented infection was also slightly higher in the Pfizer group (rarer outcomes, such as hospitalization and death, could not be assessed in this shorter timeframe because there were too few of them).
The researchers, from the CAUSALab at the Harvard T.H. Chan School of Public Health (HSPH), Brigham and Women’s Hospital, Harvard Medical School (HMS), and the Veterans Administration (VA) found that this pattern “was consistent across diverse subgroups and across periods marked by Alpha or Delta variant predominance.”
Other researchers have previously documented a higher antibody response among recipients of the Moderna vaccine, and speculated about the cause, including differences in the dose of mRNA, timing of the first and second shots (Moderna’s four-week versus Pfizer’s three-week interval) and the composition of the lipid nanoparticles used to deliver the vaccines. But “there has been a need for studies that compare the vaccines head-to-head,” write the authors, that “are large enough to provide precise risk estimates for severe COVID-19 outcomes,” that “include racially diverse groups,” are carefully designed, and that address efficacy against different variants of the SARS-CoV-2 virus.
The differences in infection rates for the two vaccinated groups were very small: the researchers estimate that there were 5.75 infections per 1,000 persons for the Pfizer vaccine group and 4.52 infections per 1,000 persons for the Moderna vaccine group during the period when the Alpha variant was dominant—a little more than one excess infection per 1,000 people. After Delta became the dominant strain, the researchers found an additional 6.54 infections per 1,000 persons in the Pfizer group.
Because both vaccines are highly effective, breakthrough cases are rare, and “either one is strongly recommended to any individual offered the choice between the two,” said first author Barbra Dickerman, a CAUSALab investigator and instructor in the department of epidemiology at HSPH. On the other hand, while the differences in estimated risk are small in an absolute sense, Dickerman adds, “they may be meaningful for larger decision-making bodies,” such as healthcare systems and governments, “when considering the large population scale at which these vaccines are deployed.”
The current study did not address the comparative safety of the two vaccines, another important consideration at both the individual and population level. “This is something we are actively investigating,” said Dickerman (whose work on a HarvardX course about causality in public health, together with senior author and Kolokotrones professor of biostatistics and epidemiology Miguel Hernan, was described in the 2017 Harvard Magazine article, “Making a MOOC.”)
Nor does it shed light on the potential efficacy of either vaccine against the new variant, Omicron, the first U.S. case of which was reported in California today. But scientists who study the virus and its vulnerabilities to known antibodies are very concerned.
Leaders of the Massachusetts Consortium on Pathogen Readiness (MCPR) addressed the many unknowns around Omicron, including its origins, transmissibility, and its ability to evade existing vaccines and treatments, in a news conference held this afternoon. Jeremy Luban, a professor in the program in molecular medicine at the University of Massachusetts Medical School who co-leads MCPR’s viral variants research program, said that during the course of the pandemic, vaccine researchers, including those responsible for developing the Pfizer, Moderna, and Johnson & Johnson vaccines, have been screening blood samples from vaccinated individuals for antibody reactivity against each of the new variants as they have appeared.
“One of the most scary things about Omicron,” Luban said, “is how many mutations it has in critical sites that are known to be targeted by antibodies.” While Delta has seven mutations in the spike, Omicron has more than 30, many of which have never been seen in patients before, but have been anticipated by scientists who have observed such mutations in the presence of antibodies during lab testing. In the scientific community, he said, “everyone is pivoting to anticipate that changes will be needed in the vaccines.”
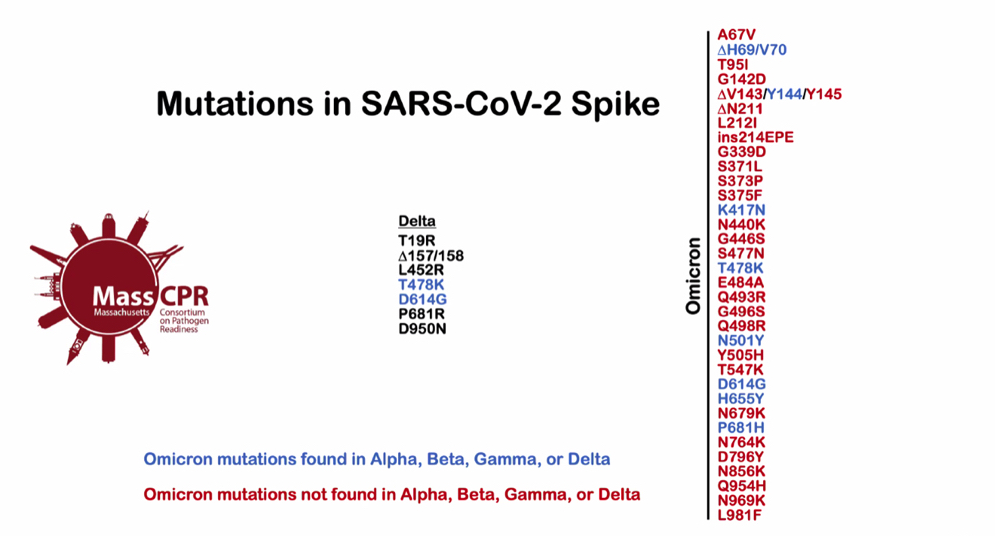
While the SARS-CoV-2 Delta variant has just seven mutations on the spike protein (used to enter cells) that distinguish it from the original strain of the coronavirus, the Omicron variant displays an extraordinary 30 mutations to the spike, most of them (denoted in red) not present in the prior variants Alpha, Beta, Gamma, or Delta—and many of them at locations known to be targeted by antibodies of the human immune system.
Image courtesy of Jeremy Luban, Massachusetts Consortium on Pathogen Readiness
It is possible that high levels of antibodies induced by the recent boosters will help despite the mutations in the spike protein that the virus uses to enter cells. And deep immune responses that rely on T-cells may also hold up, the researchers said.
But some of the COVID-19 treatments that have recently been developed, such as the monoclonal antibody cocktail from Regeneron, are reportedly less likely to be effective. Others that don’t target the spike protein directly, it is hoped, may continue to work.
Jacob Lemieux, an HMS instructor in medicine and infectious disease, and a physician investigator at Massachusetts General Hospital, noted that outbreaks like the one in South Africa that brought Omicron to the attention of the world can be driven by factors other than increased transmissibility of the viral variant, such as a superspreader event. But during the last few days, he said, the “alarmingly escalating epidemic” there, with a test positivity rate of 16 percent, increases the likelihood that Omicron will spread widely during the next few weeks and months.
Nahid Bhadelia, an associate professor of infectious disease, director of the center for emerging infectious diseases at Boston University Medical Center, and faculty co-leader of MCPR’s long-COVID program, said that one of the most important questions about the new variant—whether it causes more severe disease—won’t be known for at least a few more weeks. But she also had some potentially reassuring news: the antivirals currently being tested don’t achieve their effectiveness by attacking the spike protein, which is where Omicron’s changes lie. So “you are less likely to see an impact on them in the clinical space,” she said, “once they are approved.”
How Omicron accumulated so many new mutations is unknown, but speculation ranges from evolution in an immunocompromised individual, to a jump from humans into an animal host, and then back again, in a sort of “reverse zoonosis.” One thing is certain, emphasized Ragon professor of medicine Bruce Walker, one of the leaders of MCPR: this virus is not going away.
“We all hoped we’d be in a different place right now,” concluded Lemieux. But with respect to the path ahead, he said, “there are things we can do. Get vaccinated. Modify the vaccines. And modify monoclonal antibody treatments.”