Portraits by Stu Rosner
The next time you look in a mirror, reflect on this: the face staring back at you is literally not the same one you saw two months ago. Your skin is constantly renewing itself. Like most specialized cells in your body, skin cells are post-mitotic they cannot replace themselves by dividing. Yet there is always new skin to replace the cells that die and slough off in the shower every day. The source of the new you? Stem cells.
Doctors believe that if they can understand and harness the power of these cells, they will usher in a new era of regenerative medicine in which the body's own capacities for development and repair can be directed to cure such maladies as Parkinson's, diabetes, Lou Gehrig's disease (ALS), and heart disease. With clinical applications in mind between 100 million and 150 million people in the United States suffer from diseases potentially treatable with stem-cell-derived therapies the University announced this spring the creation of the Harvard Stem Cell Institute (HSCI), which will coordinate the teaching, training, and research of 100 scientists across 14 Harvard schools and affiliated hospitals (see "Stem-cell Science," May-June 2004, page 59). The HSCI has the full and enthusiastic support of President Lawrence H. Summers.
|
"Stem-cell transplants are already performed every day in Harvard-affiliated hospitals and around the world," says HSCI codirector David Scadden, professor of medicine at Harvard Medical School (HMS) and director of the Center for Regenerative Medicine at Massachusetts General Hospital (MGH). So-called bone-marrow transplants, which transfer tens of thousands of cells of many different kinds to a patient, most critically transfer hematopoietic (adult blood) stem cells. The proliferative capacity of these cells is so great, says Scadden, that researchers have demonstrated in mice the regeneration of the entire blood and immune system from a single cell. Hematopoietic stem cells routinely save the lives of people with diseases such as leukemia, lymphoma, and immune deficiencies.
Why is this promising area of research, with the potential to do so much good, so controversial? The seeming simplicity of the idea that there are stem cells that can generate new cells belies the complexity of the science and the ethical ramifications of its application.
The Germ of a Controversy
|
Stem cells can be either adult or embryonic. The hematopoietic stem cell (HSC), which has been known for 50 years, is an adult stem cell the only one that has been well characterized and the only one used to treat patients. Found in fetuses, umbilical-cord blood, children, and adults, adult stem cells are thought to generate only specific tissues. HSCs, for example, can create the array of cell types that make up blood and the immune system but not other organs. These blood stem cells are mostly quiescent, perhaps for months to a year, before flickering awake to divide, creating a few daughter cells called amplifiers. These amplifier cells, says Scadden, "are generally explosively prolific and have a huge capacity to divide," actively generating new tissue. But the HSCs from which they arose, because they look like any other cell and are few in number, are difficult to identify and isolate. Their deep, extended dormancies also make them hard to study or manipulate.
Most scientists believe there are stem cells for the skin, nervous system, and gut. But "not every organ and tissue in the body appears to have an adult stem cell associated with it," says Douglas Melton, Cabot professor of the natural sciences and codirector of the HSCI with Scadden. Melton is a molecular and cellular biologist who is committed to finding a cure for Type 1 diabetes, a disease that affects both his children. He recently showed that there is almost certainly no adult pancreatic stem cell by developing a "genetic-lineage- tracing technique" that allowed him to tag existing beta cells in the pancreas in order to track the origin of new cells. (Beta cells produce insulin to maintain blood-sugar levels, but in Type 1 diabetes, the immune system mistakenly attacks and destroys them.) Melton found that all new cells were generated from pre-existing beta cells. Other organs may turn out to be like the pancreas, suggesting that certain tissues cannot be generated anew from adult stem cells.
Embryonic stem (ES) cells, on the other hand, are multipotent: they can differentiate to become any tissue in the body. No other cell type is known to have this capacity. Because they are grown in a petri dish, ES cells are easy to work on. Scientists know that if they remove the inner cell mass of a blastocyst (a ball of four to 50 undifferentiated cells that forms in the first few days after a sperm fertilizes an egg), and place it in culture, some of the cells within the mass will replicate themselves in culture, indefinitely. These properties of self-renewal and multipotency not demonstrated in adult stem cells have made ES cells important for advancing the field. Scientists have studied ES cells in mice, the model mammalian system, for decades. Nevertheless, harvesting and maintaining a line of stem cells from any animal is "not routine at all," explains Andrew McMahon, professor of molecular and cellular biology. No one has been able to derive stem cells from rats, for example, even though mice and rats are closely related. So it was an astounding breakthrough when, in 1998, University of Wisconsin researcher James Thomson successfully established and sustained several human stem-cell lines in culture.
The discovery electrified developmental biologists and generated immediate controversy. Once stem cells have been harvested from a blastocyst, it no longer has the potential to develop further. President Bill Clinton, after asking his national bioethics advisory commission for a report on human stem cells, issued an executive order clarifying an existing congressional ban on the use of federal funds to create or destroy human embryos. His order did allow federal funding for research on human stem-cell lines, but not for creating them. Most researchers were satisfied that sufficient private money could be raised to create new stem-cell lines; they could then use federal money to pursue their research. But eight months after George W. Bush became president, he extended the funding ban to research on all human stem-cell lines, except those already in existence on August 9, 2001, the day he announced his policy. The apparent rationale was to prevent federal money from creating an incentive for human embryonic stem-cell derivation using private funding. Bush imposed the ban despite the fact that, nationally, fertility clinics store roughly 400,000 frozen human embryos likely to be discarded and despite the National Institutes of Health guidelines that mandated the use of such embryos in creating cell lines to be studied with federal funds.
|
"From a basic research perspective, the NIH which spends about $27 billion a year on such research is the single most important funder of biomedical science worldwide," says George Daley, HMS associate professor of biological chemistry and molecular pharmacology and associate professor of pediatrics. "So to have the NIH on the sidelines for what is arguably one of the most exciting scientific opportunities of our era is just unthinkable." Still, "When Bush made his remarkable presidential address, now almost three years ago," Daley continues, "we shouldn't forget that he fundamentally endorsed the field of stem-cell research. He realized that the work was far too important to stop altogether, even though his conservative base may have wanted him to. In fact, he went against many of his conservative advisers to promote embryonic stem-cell research. But he did it in such a way that even though the work could proceed, it was very tightly constrained," says Daley, "and I think it has had a very negative, suppressive effect on progress. Far fewer laboratories are involved than might have been had there been greater public support. It's not just the financial restriction, but the political cloud. There are a lot of scientists who just don't want to deal with the uncertainty, and so fewer scientists get engaged; fewer students get engaged."
At the time of Bush's announcement, he believed there were 60 human stem-cell lines eligible for federal funding. But to date, U.S. scientists have access to only 19.
In 1999 and early 2000, long before current concerns about the small numbers of human cell lines eligible for federal funding, McMahon and Melton worried instead about their quality. McMahon does not work with human stem cells himself, but he is an expert on mouse ES cells. He studies the signals that control developmental processes in vertebrates. These "inducing molecules" encode genetic information that triggers apparently undifferentiated cells those of an embryo, for instance to form complex structures like arms, eyes, or legs. Inducing molecules carry marching orders for the legions of cells that make up many living organisms, and they are conserved across species. So the basic research that McMahon and his colleagues have been pursuing since 1993, mostly on "precursor cells" several generations downstream from ES cells, plays a role in trying to guide stem cells to develop into specific organs and tissues, such as liver, brain, skin, or heart.
McMahon says that in 1999, he "had the view, from looking at the literature and talking with people, that there were relatively few human stem-cell lines that were freely available." He was also concerned that if the cell lines "weren't easy to work with, people might draw the wrong conclusions from working on them...and that this would lead to the end of a very promising area of research." The stakes were too high not to have good scientific tools: what was needed was "more cell lines that were better characterized, and were made readily available to anyone who wanted to work on them."
ES cells grow in culture on a layer of feeder cells and divide rapidly, forming clumps. As the clumps grow, says McMahon, the cells "tend to start to differentiate." In order to maintain a stem-cell line in an undifferentiated state, therefore, researchers must regularly break up the clumps. Some of the existing human cell lines require hand dissection to effect this a difficult and time-consuming procedure. Others are biased toward becoming a particular type of tissue, heart muscle for example, which limits their usefulness. And all are vulnerable to contamination, so they must be developed to tolerate antibiotics.
| ||||||||||||||
McMahon and Melton therefore resolved to create new human stem-cell lines that would be easy to break up and disperse (using a topical enzyme), that had no bias to become a particular tissue, and could be grown in the presence of antibiotics. And in contrast to the "presidential" cell lines that now cost as much as $5,000 apiece, they decided to distribute their cell lines free to any qualified researcher. The Howard Hughes Medical Institute funded their proposal, and McMahon helped design a fully self-contained, Harvard-donated laboratory to ensure that there would be no violation of federal funding rules. But his key contribution, he says, was realizing that the best person to create the new cell lines was "the person who had done most of the derivation of new embryo stem-cell lines in my own lab, and that just happened to be my wife" staff scientist Jill McMahon.
Together with Douglas Powers, chief scientific officer of the private fertility clinic Boston IVF (which provided the frozen embryos and helped set up the embryology culture lab), Jill McMahon worked part-time with Melton's group for a year and a half, starting in 2001. They began with 344 frozen embryos, most just 6 to 12 cells each, all donated knowingly for research by couples who had ended treatment and had already indicated that their remaining embryos should be discarded. The group's work culminated in the announcement this spring that 17 new stem-cell lines were available, more than doubling the supply then available to U.S. scientists and prompting more than 300 requests for the cells so far.
Transplant Therapy: The Way Forward
Given good tools like these cell lines, how might scientists use them to pursue clinical applications? There is more than one path to a cure for any disease, and that is perhaps especially true within the field of stem-cell research. The approach most widely discussed in the press is that of tissue transplant. Bone-marrow and organ transplants make that approach easy to explain and understand. But can it work?
"We have to ask ourselves two critical questions," says Andrew McMahon. "How does a particular tissue normally form, and what are the properties of the organization of that tissue that [must] be taken into account if we were to use tissue-based therapies derived from stem cells?"
Type 1 diabetes, the problem that concerns Melton, is well-suited to stem-cell therapy. It involves a single cell type, the beta cell, that is either missing or present in numbers too low to regulate blood-sugar levels. "If you could place that cell type back into a person [so] that it was not subjected to autoimmune attack, where it could be healthy and thrive, even outside the context of the pancreas," says McMahon, "then you could cure diabetes." One current therapy for Type 1 diabetes the Edmonton protocol involves injecting beta cells from three cadavers into a patient's vein; the cells seed the liver and work from within that organ. But nonsteroidal immunosuppressants are required to control both autoimmune attacks and rejection of the foreign cells by the patient's body. Nevertheless, a first test of beta cells created through directed differentiation of human ES cells might be to use them in the Edmonton protocol. The next step might be to create a device beta-cell tissue grown on a synthetic three-dimensional biomatrix and encapsulate it in a Gore-Tex-like membrane that would allow glucose and insulin, but not immune cells, to pass through. Separate stem-cell therapies (see below) hold the promise of completely stopping the immune attack.
|
The structural and functional simplicity of organs like the pancreas or the liver make them relatively easy to mimic, and scientists already know the signals that vascularize tissue, so getting a blood supply to a transplanted organ is not an obstacle. But what about a complex organ like the kidney? "The kidney has at its core a long convoluted tubule, the nephron, and a very precise architecture of vascular input and a shape and organization of the structure that is critical to its function," says McMahon. "To recapitulate all of that would be tricky." Furthermore, making an organ is not the same as maintaining it the kidney doesn't have to function in an embryo while it is being built. In addition, says McMahon, "the scale on which you have to remodel and regenerate structures is [one at] which those events never normally occurred during the development of the embryo." The wiring of the body's central nervous system presents a similar challenge. "You can imagine how connections between neurons are established over a few millimeters," he says, "but when you think about how you regenerate circuitry over the scale of an adult brain, it's a different order of magnitude." A single nerve cell that allows you to sense something in your toe might be the length of your leg, but it formed over the distance of a few millimeters and then grew.
The problem is not just one of distance, but also environment. Cells are acutely affected by their context. In an embryo, ES cells are nothing more than a transient cell type lasting perhaps a day or two. But if they are removed from the embryo at just the right stage of development and placed in a petri dish, they self-replicate and become, in essence, immortal. If those same ES cells are put into an embryo, they will develop normally to become a whole animal but if they are injected into an adult, they will form a cancerous tumor. In other words, getting cells to differentiate into beta cells in a petri dish doesn't necessarily mean they will thrive as a stable beta-cell population when transplanted into a patient.
Despite this complication, stem-cell therapies have distinct advantages over other approaches in certain diseases. That is because many cellular diseases are polygenic (many genes, perhaps in many combinations, can cause them) and multifactorial (external environmental factors perhaps simple changes in food, water, or air can determine whether someone is affected). Type 1 diabetes is a classic case. "There are probably 10 to 50 genes that give you a predisposition to get the disease," says Melton, "but even if you have all of them, you might not get it. There are identical twins who have the same genes, only one of whom has the disease." That means knowing the human genome, or even the genes involved in the disease, may not help much to cure diabetes, says Melton. From a cellular perspective, though, the disease is simple: one missing cell. "And that is what we would be putting into people."
But there are two utilities to these cells. "One is the cell itself, as a product," says Melton. "The other is [learning] how to get these cells to differentiate. If we discover new chemicals or genes that do this, that...could be used to have patients heal themselves. It's a broad area of research into replenishment and regeneration, and getting cells into patients is not the only form of success."
Awakening the Cells Within
A group led by David Scadden at MGH is actively working on strategies using chemical and genetic signals to encourage hematopoietic stem cells to proliferate in the body. Some approaches have already been approved for clinical studies.
The ideal bone-marrow transplant, says Scadden, is autologous: stem cells are harvested from patients, then frozen; the patients' disease is then destroyed along with their blood and immune systems; and patients are then transplanted with their own blood. But this procedure doesn't work for everyone. Ten to 20 percent of patients, either as a result of their disease or prior treatment, simply don't have enough blood stem cells for a transplant to work. "If we could make a difference there," says Scadden, "that would be enormously valuable."
When a genetically matched bone-marrow transplant is needed, as in leukemia or when an autologous transplant has failed, doctors turn to donor registries. Unfortunately, "not all ethnic groups donate," says Scadden "and that leaves some people with a very poor chance of finding a donor." However, there is a "wonderful resource" in umbilical-cord blood banks that could "overcome this problem." When umbilical cord blood which would otherwise be discarded is donated instead, the donations have created banks where physicians can find a match for just about anybody. The problem is that cord blood "doesn't have enough stem cells to safely transplant into an adult," Scadden explains, "so if we could find ways of either needing fewer stem cells or being able to expand [their numbers], that would be a tremendous asset and change transplants as we currently do them."
The problem is that HSCs are deeply quiescent and don't respond easily to any kind of signal. This probably keeps them from exhausting themselves, and also guards against rampant proliferation that might lead to cancer. So how can they be stimulated? Scadden and HMS professor of medicine Henry Kronenburg, who also works at MGH, have hit on a new strategy: reach the stem cell by changing the environment where it lives.
|
During early development, blood-forming HSCs are found in three different locations, and in each place, they "behave a little differently," says Scadden. "Location clearly has a relationship to function." Because scientists know that HSCs in adults live in the marrow, very close to the bone, they decided to try to manipulate specific elements of bone physiology, using mice, to see how stem cells would be affected. Genetically engineered mice with an increased number of bone-forming cells called osteoblasts also showed changes to their stem cells. Having effected changes in the stem cells with a genetic approach, researchers then tried applying a hormone that has the same effect. That also worked, which was intriguing because "the stem cell doesn't see the hormone and doesn't respond to the hormone," says Scadden. "The stem cell instead responds to something that's changed in the bone..., the microenvironment or the niche where the cells live."
"We then put the mice through a bone-marrow transplant," says Scadden, "but gave them too few stem cells," modeling what might happen if you transplanted an adult human with cord blood. The hormone had a dramatically positive impact not by increasing the rate of cellular proliferation, but by changing stem-cell division itself. Instead of making one copy of itself and one daughter cell during division, stem cells in the hormonally altered environment tend to create two copies of themselves, thereby doubling their numbers. Because the hormone is already approved for treating osteoporosis, the Food and Drug Administration quickly allowed testing the treatment in patients who can't otherwise find marrow-donor matches.
Scadden is also working on genetic techniques to suspend temporarily the quiescence of adult stem cells, increasing their rate of proliferation. Using a method of changing messenger RNA discovered by Melton, Scadden has been able to deliver genetic instructions to adult stem cells that remove the molecular brake that keeps them from dividing frequently. Using mice that had undergone a stroke, the scientists found that when the molecular brake was removed, the animals created more new neurons. "That suggests," says Scadden, "that if you could unleash some of the stem cells in a setting of injured tissue, you might be able to improve repair." Such stem-cell expansion might be useful, he says, "not just for blood disorders, but potentially also in other disease types."
Cancer, See-through Fish, and Drug Therapies
Like Scadden, HMS professor of pediatrics Leonard Zon, a hematologist at Children's Hospital, focuses on studying blood formation. He is president of the International Society for Stem Cell Research and a strong believer in the power of collaborations such as the HSCI to advance the pace of research discovery. One of the goals of his work with zebrafish is to understand all the genes that contribute to blood formation. Another is to understand how cancer develops.
|
There are molecular similarities between stem cells, which have the ability to self-renew, and cancer cells, which have acquired the ability to self-renew, says Zon. "If I transplant a stem cell, it reconstitutes the immune system. If I transplant cancer, some of the cancer cells will recapitulate the disease. I can take cancer out of one mouse and put it in another mouse, and that mouse gets cancer." But some tumors are heterogenous, says Zon, meaning some cells can metastasize and others cannot. Understanding that heterogeneity, he suggests, "is a useful concept, because you may want to treat the stem-cell part of the disease of cancer, rather than the whole cancer." This is the sort of question that might be probed with tools like the "genetic lineage tracing" technique developed by Melton to track the origins of beta cells.
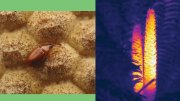
The zebrafish embryos Zon uses for his blood and cancer research are transparent, allowing him to study the blood cells and vasculature in vivo under a microscope. Using time-lapse photography, he can actually watch the cells reconstitute the immune system after a marrow transplant. He collects zebrafish with diseases, clones the genes responsible for the disease, and uses them to find the human versions. In one case, working with a mutant zebrafish that had very few blood stem cells, Zon's group discovered a gene that controls blood-stem-cell production in the embryo. In collaboration with his colleague George Daley, Zon then inserted the gene into mouse embryonic stem cells and found that it directed them to make blood stem cells a key step toward actually making HSCs that could be used for transplantation. Zon is now seeking a drug that will mimic the action of the gene and convert embryonic stem cells into HSCs.
|
Using his genetic approach, he adopts three general strategies for curing disease. One is to use gene-therapy equivalents, thereby giving back the normal version of a mutated gene. Another approach is to enhance a separate gene in the disease pathway. "A gene is usually part of a pathway that goes from gene A to gene B to gene C," Zon explains. If B is mutated and therefore not working properly, "we might be able to overexpress the C gene, and perhaps rescue the pathway." A third possibility is to find small molecules drugs that could prevent the disease phenotype.
This last approach demonstrates one of the advantages of working with mutated fish: Zon can create huge numbers of them to test various chemical compounds. One of his fish strains has very high rates of cancer caused by a severe cell-division problem. Hoping to find a drug that would correct this genetic disease, his lab mated 100 pairs of fish over four months, producing 3,000 embryos a week. He put the embryos in wells, and then tested 16,000 individual chemicals in the various wells. One cured the disease.
Human ES cells can provide a way to perform the same kind of large-scale experiments using a human model of a disease. Given human ES cell lines with specific diseases, scientists could create thousands of diseased cells against which to test thousands of compounds. By using an embryo identified, through pre-implantation genetic diagnosis, as having a genetic disease, one could derive stem cells that would carry the genetic defect.
Toward Therapeutic Cloning
An even more effective approach, because it would capture more diseases (not just those for which there are simple genetic screens), would be to create new human ES cell lines from diseased patients using a technique called somatic cell nuclear transfer (SCNT). By inserting the nucleus of a cell, say a skin cell, into an egg that has had its nucleus removed, scientists can create an embryo that has almost all the same genes as the skin-cell donor; only the mitochondrial DNA, which is passed in the maternal line through the egg, would be different. They could then derive an embryonic stem-cell line from the resulting blastocyst and use the cells for research or, eventually, to create histocompatible cells for the diseased patient. The result: no immune rejection.
This is the technique, called either therapeutic cloning or cloning for biomedical research, that was demonstrated in humans for the first time this spring by South Korean scientists. Although controversial it involves taking the same first steps used to clone an adult animal (like the famous sheep, Dolly) it also opens the door to tremendous therapeutic applications. (The International Society for Stem Cell Research to which all the Harvard stem-cell scientists belong supports therapeutic cloning but urges a ban on human reproductive cloning.)
Immuno compatibility problems plague tissue- and organ-transplant recipients. George Daley, Zon's office neighbor, is trying to use stem cells to control or eliminate this immune attack. One strategy, he says, might be to create "universal donor cells" from ES cells. In theory, pure HSCs, when transfused into a patient whose own immune system has been irradiated, would not create histocompatibility problems. If one could create HSCs from an ES cell line and transplant them, "this would establish your tolerance to any of the tissues coming from that ES cell," says Daley. "If I wanted to make a neuron or a pancreatic beta cell or a cardiomyocyte, I could give them to you and you'd tolerate them without immune rejection." Another way to create universal donor cells, he says, would be to "replace the immune genes of those ES cells with immune genes from the patient we wanted to treat"; that, too, would in theory create customized cells for therapy.
|
But the alternative for dealing with immune rejection that Daley favors is SCNT, creating a "novel embryonic stem-cell line that is uniquely customized to you, the individual patient." He has actually used this approach to perform a stem-cell transplant that cures disease in a mouse. "We started with an immune-deficient mouse that is a model of Bubble Boy disease," he explains. "The mouse lacks a gene that is required for formation of the immune system, so [it has] no B cells and no T cells." Then he takes a cell from the mouse's tail and transfers its nucleus into an egg from another mouse whose own DNA has been removed from the egg. A few days later, a blastocyst-stage embryo develops. Daley removes the inner cell mass and generates an embryonic stem-cell line, just as Melton did, except this one is coming from a cloned nucleus. The cell line's DNA is genetically identical to that of the first mouse, and therefore carries the same genetic defect.
"Using a very simple technique," says Daley, "we can then repair the genetic defect in that cell with surgical precision." This is not the version of gene therapy, using a virus to deliver DNA to a living subject, that "runs the risk of activating genes, or inactivating genes, that you don't want mucked with." The advantage of Daley's homologous recombination, as it is called, is that it allows normal DNA to be added to a cell in a petri dish, where it lines up with the mutated gene. The normal gene is exchanged for the abnormal gene, and then Daley grows the resulting cell and "characterizes" it, verifying that the defect has been corrected.
Daley is also working to cure a sickle-cell-anemia-like disease in mice using this therapeutic-cloning technique. He says it could be used for any genetic disease of the bone marrow and ultimately leukemia. But the work must be duplicated with human cells.
"We could work for years on mouse models," continues Daley, "and become very elegant and effective at curing mice. I am trained as a physician; I practice as a physician. I see a huge unmet medical need for treating patients with diseases of the blood and bone marrow....Many of the bone-marrow diseases are diseases of kids," he says, "or diseases that would otherwise kill or cause horrendous chronic diseases in children. If we really want to treat patients, we learn the most from studying human cells."
Jonathan Shaw '89 is managing editor of this magazine.