Last spring brought alarming reports of the first known case of a germ resistant to colistin, considered an antibiotic of last resort. The bug, a strain of E. coli, was found in a culture taken from a Pennsylvania woman with a urinary tract infection.
Thomas Frieden, director of the Centers for Disease Control and Prevention, responded by warning that “the medicine cabinet is empty for some patients,” with few new antibiotics in development to fight drug-resistant super bugs. As of 2013, only four international pharmaceutical companies were still attempting to produce new options; in May, The Economist noted that, given the expense of drug development, companies prefer to focus on medicines for chronic diseases such as high blood pressure, which patients take indefinitely.
The Pennsylvania woman’s infection happened to respond to other existing antibiotics, but the failure of colistin renewed conversation about the dangers of multiple-drug-resistant infections and the startling lack of remedies (discussed at length in the feature “Superbug: An Epidemic Begins,” May-June 2014, pages 40-49).
The dearth of new treatment options led Andrew Myers, Houghton professor of chemistry and chemical biology, to create with his students a platform that may speed the process of developing macrolide antibiotics. “Macrolide” means “large ring,” and describes the circular chemical structure of this class of antibiotics. These popular drugs are generally well tolerated by patients, but increasingly ineffective against a range of bacteria, Myers explained in an interview.
His method uses eight commercially available chemicals, or substances derived from them, to make building blocks that can be assembled into new ring-shaped molecules. The molecules are then tested for their ability to fight pathogens. In a research article published in the journal Nature, Myers and his colleagues (including postdoctoral fellows Ian Seipel and Ziyang Zhang) reported that they used the method to construct more than 350 new compounds. “The majority of those compounds had antibiotic activity, and two had activity against clinical isolates with fierce combinations of antibiotic-resistance mechanisms,” Myers said.
These new molecules are fully synthetic, unlike the first macrolide, erythromycin, which was discovered in a soil sample from the Philippines in 1949. “That was the post-penicillin era, a time when many pharmaceutical companies were scouring the globe, looking for new natural products that might be antibiotics,” Myers pointed out.
Erythromycin was approved for human use in 1952, just three years after the initial discovery—a rapid pace unheard of today, Myers noted. After that, scientists seeking new antibiotics often started with the erythromycin molecule and carried out “one or more chemical reactions to change the structure, but not in a drastically different way,” he explained. This approach, known as semi-synthesis, “has dominated discovery of new antibiotics in this and other classes for many decades.”
His team, instead, has built its molecules “from the ground up.” The researchers determined that they could break the macrolide molecule into eight modules, or building blocks, that could be made from the commercial chemicals. The next step—a challenging one—was to map ways to reassemble the modules into macrolides. His students, he said, “worked very hard to identify chemical reactions that would allow us to link the building blocks in the precise way that was required, in some cases even inventing new transformations.”
The modular approach eliminates the difficulties of working with erythromycin, a complex natural product. “It is very challenging to conduct chemistry specifically and efficiently on just one portion of the molecule without affecting others,” Myers explained. “By building from scratch, it is possible to modify just about any position of the molecule that one wants.”
The lab continues to make new macrolides by systematically assessing different chemical combinations, and then testing them against a panel of bacteria, including drug-resistant super bugs. “We’re going to have to make a lot more molecules before we’ll find what might be a drug candidate,” Myers added. Any promising molecule that emerges will face an arduous and expensive process lasting a decade or more, including preclinical animal studies and three phases of human studies before it reaches the Food and Drug Administration for regulatory approval.
This research builds on similar work the lab undertook to develop new tetracycline antibiotics, which led his team to found Tetraphase Pharmaceuticals in 2005. The company has made several thousand synthetic tetracycline molecules, including one drug that has completed a phase 3 trial.
But funding this research has been difficult: “In my experience, there is no money coming from the National Institutes of Health to support actual antibiotic discovery,” Myers said. He has run these projects on smaller grants from Alastair Mactaggart ’88 and his wife, Celine, the Gustavus and Louise Pfeiffer Research Foundation, and Harvard’s Blavatnik Biomedical Accelerator. Last year, he founded Macrolide Pharmaceuticals to commercialize the new process.
Myers is motivated to continue pushing toward new drugs. “This is a scary situation,” he stressed. “People talk about going backward to a pre-antibiotic era where you could go in for knee replacement surgery and lose your leg, or even your life, to an infection. I hope it won’t come to that.”
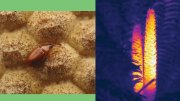
In separate work, researchers from Harvard Medical School and the Technion-Israel Institute of Technology have shown just how quickly drug resistance can arise in a population of bacteria. A video (below) produced in the lab of HMS visiting professor of systems biology Roy Kishony shows how such resistance develops: during the course of just 11 days, E. coli in a rectangular growing medium—prepared with progressively higher gradients of an antibiotic—mutate to eventually became resistant to the highest concentrations of antiobiotic. The video above documents the rapidity of this microbial evolution, while the accompanying Science paper demonstrates that resistance to low-levels of antibiotic acts as an evolutionary stepping stone to high levels of resistance.
Video courtesy of Kishony lab, Harvard Medical School and Technion - Israel Institute of Technology
The Evolution of Bacteria on a "Mega-Plate" Petri Dish from Harvard Medical School on Vimeo.