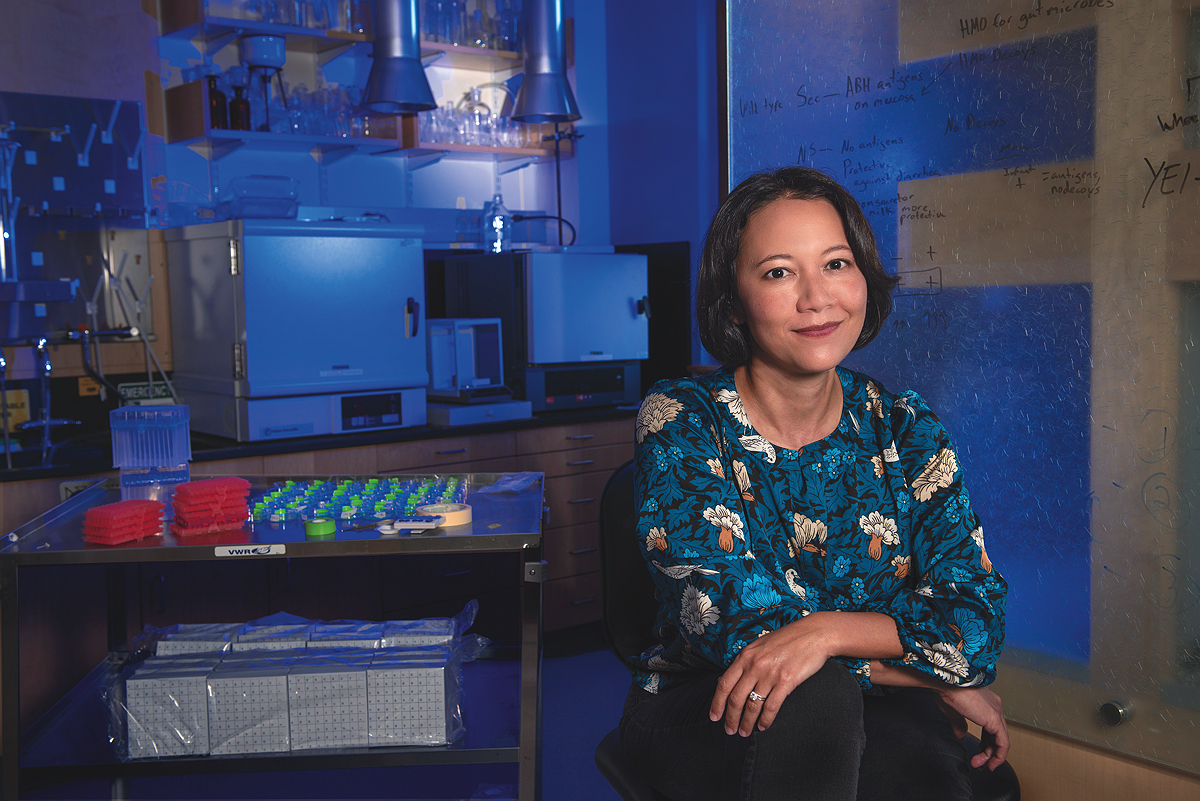
In the late 2000s, Rachel Carmody was spending a lot of time counting calories. An anthropology graduate student at Harvard, she was studying whether cooking changed the number of calories the gut can extract from food. When humans invented cooking thousands of years ago, she and her advisor Richard Wrangham wondered, had they opened the door to a new source of energy?
To find out, she’d fed raw or cooked food to mice and humans. She’d checked on the food in mice as it traveled through the stomach, the small intestine, and the large intestine. She’d even recruited people whose colon, a portion of the large intestine, had been removed, to take samples from their ileostomy bags so she could see what the food was like. She compared the energy that went into their bodies with what came out. And she and Wrangham discovered something extraordinary.
Cooking dramatically increased the calories humans and mice got from food. Cooked meat yielded 10 to 15 percent more calories than raw. Cooked sweet potatoes were a whopping 30 percent more caloric than uncooked ones. Now, in her office in the Museum of Comparative Zoology, Carmody, an assistant professor of human evolutionary biology, recalls her hunt to understand why.
Here’s part of what she found: cooking jump-starts digestion. With chemical bonds and cellular structures already broken down, it’s easier for digestive enzymes to make the energy in food available to an animal. But she could account for only a portion of the energy boost cooking produced. “I was panicking that my dissertation was going to be terrible,” she says. Something was missing.
Meanwhile, biologists at Washington University in St. Louis and elsewhere had been learning that diet could alter the gut microbiome. What’s more, those bacteria, fungi, and viruses that live mostly in the large intestine and feed on molecules the host can’t break down seemed to be giving energy back to their hosts. As Carmody learned more, she understood that those microbes might hold the answer. If cooked food changed the microbiome, then the microbiome might help explain the perplexing caloric power of cooked food.
It was a hard sell. “Nobody in this department, at that point, cared about the microbiome,” she says with a smile. “I was the weird grad student constantly talking about bacteria.” But she couldn’t leave the idea alone. “If the microbiome was, in fact, interacting with us and our diet in that way,” she continues, “this was not just having an impact on how many calories we were getting out of meat, or a tuber, or a peanut. This was changing everything about our biology.” She and Wrangham had begun investigating cooking in the first place because they suspected better access to energy might have enabled the evolution of the oversized, energy-intensive human brain. Could the microbiome—something that few of her colleagues knew much about—have shaped human evolution? And could it be shaping aspects of our health today?
One morning she woke up and realized something even more profound. “I am a human evolutionary biologist who doesn’t actually know what a human is,” she remembers thinking. The borders between humans, their inhabitants, and the diets of both seemed suddenly flimsy. She didn’t know where the organism ended and the rest of the world began. It’s a kind of vertigo that has propelled her through more than a decade of scientific work and made her one of the most promising young researchers studying the microbiome. “I decided that day,” she says, “I had to study this.”
“We Can Test This”
Carmody did not start her professional life as a scientist. When she was an undergraduate at Harvard in the class of 1999, she thought she might study English. A human behavioral ecology class taught by Irven DeVore helped make her an anthropology concentrator. “I got absolutely hooked on the idea that so many of the unique quirks that I could observe in myself and in the humans around me made sense in light of biology,” she says.
But after her junior year, while studying primates in Uganda’s Kibale National Park, Carmody rethought her plans to attend graduate school. It was immediately after the Rwandan genocide. “Some of the people who were responsible for it were hiding out in the forest that I was living in,” she says, driving by on trucks, out of reach of justice. She realized, suddenly, how little she still knew about the world. Growing up in Hawaii, way out in the ocean, she had not had many opportunities for international travel. And so, she decided to find a way to get paid to see the world. After graduation, she took a job as a management consultant with Oliver Wyman.
The work was engaging and challenging, and she got her wish, traveling almost continuously for six years. However, she found that at night, she was reading about human evolution. “I had this realization that if I didn’t leave now, I would never leave. And I would regret not having pursued the thing that I was really interested in,” she said. She quit that week.
In graduate school, she arrived just as Richard Wrangham (now Moore research professor of biological anthropology) was pondering deep questions about humans and food. “People had done very little to investigate carefully the impact of the invention of cooking on the evolution of humans,” he says. He suspected the field was overlooking one of the most important factors in the development of the genus Homo.
Carmody recognized a problem she could tackle right away. While researchers debated whether cooked food was nutritionally different from raw, she leapt into action. “She said, ‘OK—we can test this.’ And off she went and did it,” Wrangham says. She not only learned how to perform physiology experiments with mice and people but delved into the chemistry of fat, proteins, and carbohydrates to understand how cooking changed them. She was able to show, in a sweeping finale, that the genes humans use to digest cooked food show signs of being under positive selection, meaning evolution had favored their spread. “She was astonishing,” says Wrangham, whose popular book, Catching Fire, draws on the work he and Carmody did together.
In a matter of a year or two, she’d gone from not understanding what a human was to the conviction that, to discover the answer, she would need to start from scratch in a new field.
But studying the microbiome, as she decided she had to do, meant leaving anthropology. After earning her Ph.D. in 2012, Carmody turned down a prestigious job and joined the lab of Peter Turnbaugh, a microbiologist and former Bauer fellow at Harvard’s center for systems biology who had joined the University of California, San Francisco. In a matter of a year or two, she’d gone from not understanding what a human was to the conviction that, to discover the answer, she would need to start from scratch in a new field.
The Microbial World
The human gut microbiome is many things. It includes microbes we inherit from our mothers during birth, swallowed on the way through the birth canal, and microbes from breast milk and the mother’s skin that are ingested within the first month. The microbiome dines on substances in breast milk that the infant’s short intestine cannot break down. Of these there are a startling number, suggesting that long ago, evolution might have selected for milk that feeds a population of bacteria, viruses, and fungi, as well as a child.
The microbiome is strangely immovable. Adults who eat yogurt loaded with living bacteria do not change the composition of their gut microbiome for the long term. Newcomers, should they survive the acid bath of the stomach, are confronted with an established community with little space, scientists believe. But the microbiome is fragile. When antibiotics are given to infants to fight bacterial infections, the drugs change the types of bacteria present in the gut, an effect that may last for months or even years.
Although made up largely of bacteria—the same class of organisms that can sicken us—the microbiome is safe, even necessary for health. Scientists now believe that gut microbes train the human immune system in ways they don’t fully understand, perhaps helping to prevent allergies and autoimmune conditions. But the microbiome can be dangerous. Use of antibiotics can breed drug-resistant strains like Clostridium difficile, a bacterium that spreads quickly through the guts of hospital patients and provokes severe colon damage. Fecal transplants, in which feces from a healthy donor are placed in a patient’s colon to try to replace a microbiome ravaged by C. difficile or another microbe, have shown promise. But sometimes the donor’s bacteria are perilous as well: In one trial, a patient died when a donor’s microbes included a drug-resistant strain of E. coli.
This kaleidoscope of paradoxes has drawn a growing community of researchers to the study of microbiomes, both in the human gut and elsewhere. “Arguably, the biological field is at one of its greatest inflection points since Charles Darwin introduced the theory of evolution,” says Seth Bordenstein, a professor of biology at Pennsylvania State University. “[It’s] because of the recognized interest and appreciation of the microbial world in ways that we could not have imagined before.”
Carmody had a lot to learn when she began to work with Turnbaugh. In his lab, she learned techniques like raising mice that lack a microbiome of their own in order to give them a human one and using DNA sequencing to identify what strains are living in a particular gut. In her graduate work at Harvard, she had already contributed to research showing that changing the contents of one’s diet—by eating more fiber, for instance, which is digested by the microbiome rather than by the host—was a more effective way of altering the microbiome than eating microbe-rich foods like yogurt. But when she’d been in San Francisco less than a year, she learned of a job opening in her old Harvard department studying human evolution, diet, and the microbiome. She applied, thinking of it as practice.
“We’re always a little bit skeptical” of hiring scientists who were graduate students at Harvard, says Lerner professor of biological sciences Dan Lieberman, who is interim chair of the department of human evolutionary biology. It’s more common to hire outsiders who can bring in fresh ideas.
“But Rachel is exceptional,” he says, citing her uncanny ability to identify promising experimental questions and her highly unusual skillset to pursue them. Carmody can collect fecal samples from wild chimps, brainstorm experiments where mice run on wheels and eat raw diets, conduct genetic analyses, and dissect the biochemistry of individual carbohydrates. This breadth enables her to start with observations of the natural world and drill all the way down to the molecular mechanism that underpins what she sees. “She opens the black box,” Lieberman says. “It’s really the mark of a great scientist.”
Offered the job, Carmody worried she wasn’t prepared. She arranged to defer the appointment until she had finished two years at UCSF. In 2016, she returned to Harvard to start her own lab.
The DNA in Dinner
One morning earlier this year, the sunny rooms of Carmody’s lab space were stacked with pipette boxes. In her office, whiteboards covered with her neat handwriting attest to the lab’s open questions. She is still working to understand what cooked and raw foods do to the human microbiome. In 2019, she, Turnbaugh, and collaborators published a study focused on human volunteers who ate two specially designed menus—prepared by Vayu Maini Rekdal, a graduate student who was a former chef—that differed only in whether the ingredients were raw or cooked (it was a kind of logic puzzle to pick dishes that worked either way; winners included chia seed puddings and pea and sweet potato patties).
They saw that the two diets did provoke different changes in the subjects’ microbiomes. In further experiments with mice, they discovered that endowing mice with a microbiome adapted to digesting raw food made them plumper than mice whose microbiomes had been trained on cooked food. Could it be, Carmody wondered, that the community of bugs exposed to raw food, with its less abundant calories, was poised for a time of scarcity? Could the microbiomes of early humans have provided a kind of buffer against starvation? Perhaps, primed by scarcity, the microbiome of those who’d gone hungry might have been better adapted to seize energy from what food was available, allowing a host to glean more from the environment. Pursuing these ideas, Laura Schell, a graduate student in the lab, is now studying another version of this situation: how early-life exposure to antibiotics—a form of stress for the microbiome—might prime microbes to hang on to energy later in the host’s life, leading to greater risk of obesity.
Another of the angles Carmody is exploring, inspired by her Ph.D. work with Wrangham, employs a technique called DNA metabarcoding. She wants to understand just how each piece of food that a mouse, chimp, or human ingests interacts with the gut. When you eat a given diet, what parts are feeding your microbes, rather than you? How much of that spinach leaf, for instance, makes it to the large intestine? “When you’re studying these diet-microbe interactions, and how the diet is shaping the microbiome, you really want to account for what actual fraction of the diet the microbiome is seeing,” says Emily Venables, a graduate student in the lab who is using this technique.
So, before a subject takes a bite, Carmody, Venables, and colleagues sequence some DNA from the food item. By looking for those sequences again in partially digested food taken from an animal’s gut, they can deduce what foods have already disappeared by the time the meal reaches the microbes. By looking for them again in feces, they can see how much has disappeared over the course through the whole gut, and perhaps ask questions about why some things are left.
Already the approach has shed new light on work Richard Wrangham and colleagues have long pursued with chimps in Uganda. For decades, researchers have closely recorded the plant and animal species that make up their diet. But using DNA metabarcoding, Carmody, Wrangham, and colleagues found that there were species in the chimps’ feces that had never been recorded in their diets. When a chimp grabs a handful of vegetation to eat, Carmody suggests, there’s more than just the obviously visible plants in that fistful. There are microscopic fungi, tiny plants, perhaps even parasites—a huge collection of things that might be important to our nearest ape relatives.
The team has confirmed that what goes into the colon is a better predictor of what will happen to the microbiome than what goes into the mouth, Carmody notes. Understanding just what disappears before it reaches the bugs will help researchers grasp how and why diet shapes the microbiome.
In the process of pursuing these questions, Carmody contends with issues surrounding the microbiomes of today. The gut microbiomes of people who live in the developed world are less diverse than those of modern hunter gatherers, like the Hadza of Tanzania. Residents of developed nations also have higher rates of autoimmune and inflammatory diseases and problems like obesity and heart disease. Some researchers have posited that microbiomes may be contributing, perhaps by creating a mismatch between what the human immune system evolved to encounter in the gut and what’s there today. Missing Microbes, a book by Martin Blaser, a professor at Rutgers University, explores the possibility that the microbiome humans develop when they are young children may play a powerful role in contemporary diseases. “That’s the microbiome that is involved in programming things like metabolism, immunity, and cognition,” he said in a recent interview.
These observations have led some to suggest that “rewilding” the microbiome—somehow resetting it by introducing new strains—might be helpful. But that idea could lead to unintended consequences, because few of the important details (including where this microbiome would come from) have been worked out. It’s not clear that the microbiome of our ancestors was similar to that of modern hunter-gatherers. And there’s a need for stronger evidence of a connection between lower microbiome diversity and health outcomes, too, says Carmody. “We do see correlations between disease states and low diversity. But we never know whether low diversity promotes disease or whether having a disease then causes the body to lose [microbial diversity]. So, we don’t know even something as simple as, ‘Is diversity beneficial?’”
What’s more, although there has been much discussion of how modern lifestyles might harm the gut microbiome, there has been little mention of whether those bugs—so potentially mutable—might be adapted to them. In other words, Carmody posits, the microbiomes we have now might be helping people deal with the conditions present in the contemporary world. Could it be that the ability of the microbiome to adapt to its present circumstances helps humans in ways previously unnoticed? She has set out to study the problem, using mice equipped with various human microbiomes.
“The number one question that I get is, so what should I be eating?”
The composition and effects of their personal microbiome and whether it can be helpfully altered remain vague for most people. “The number one question that I get is, so what should I be eating?” Carmody says. “My honest answer back to them is, well, it depends what microbiome you’re targeting. And we don’t know what a healthy microbiome is.”
But some of what she and other researchers have learned suggests that, in the future, knowing what lives within a human could influence medicine profoundly. Sitting in her office, having sketched the sweep of human evolution and discussed chimps and mice in equal measure, Carmody returns to that nearly invisible separation between the body, the microbes, and what they eat.
She notes that among the substances altered by a patient’s gut population are the medications they take. “Most of the common drugs that are out there in the world do interact with the microbiome—either they change the microbiome, or the microbiome changes them, or the microbiome changes the way that hosts metabolize those drugs,” she says. (Drugs with documented effects on the microbiome include many antidepressants.) When she was in Turnbaugh’s lab, Carmody helped raise awareness of the role the microbiome can play in drug metabolism, and she continues to be interested in the subject. One recent study that fascinated her traced the variation in how people respond to a Parkinson’s drug back to their gut microbes. Different amounts of the drug reached their brains, depending on the different ways patients’ gut microbes metabolized it. (The work was performed by Rekdal, the graduate student who collaborated with Carmody on the raw and cooked food study, and Carmody’s fellow faculty member Emily Balskus, Cabot professor of chemistry, and colleagues [See “The Sleuth,” July-August 2021, p. 36].)
“That’s a simple example of how, if you knew what bugs were in a person’s gut, you could adjust their dosage,” Carmody says. A physician could someday predict whether a particular individual needs, say, 20 percent more or 50 percent less of a medication in order to standardize the dose that is reaching the brain, she continues. Each drug, each set of interactions with specific microbes, would need to be determined in order for this vision to become reality. But, says Carmody, in her characteristic matter-of-fact manner, it’s doable.
“I’m addressing a lot of basic questions,” she says of her work: what the microbiome eats, how environmental factors influence it, how it feeds the body in which it lives. “But all of the work that we do ultimately has a health impact as well.”
“The way we see microbiome science 20, 30 years out is really as an individualized tool,” she says. “There is tremendous potential.”