One story David Mooney tells starts with a slug. “This slug does a really good job of creating a mucus that allows it to stick really tightly, so predators can’t just peel it off and eat it,” he says. The mucus, a marvelous material, turns out to consist of a springy mesh made of sugars and proteins threaded through each other. When pushed with a finger, the energy disperses through the mesh, rather than tearing it, indicating serious toughness. There’s plenty of water in there, too, Mooney points out. That’s handy, because if you want a substance to stick to your inner organs, it’s more convenient if you know it can withstand the damp.
Mooney is not a slug biologist. He is in fact the Pinkas Family professor of bioengineering, a founding faculty member of Harvard’s Wyss Institute for Biologically Inspired Engineering, and the holder of numerous patents on subjects ranging from recipes for cancer vaccines to ways to guide drugs through the body (see “Fighting Disease in Situ,” May-June 2009, page 10, and “Biological Vaccine Factories,” January-February 2021, page 9). But he is a strong proponent of observation. One researcher in his lab realized that the slug mucus strongly resembled material another group member had been exploring some years before. Then two post-doctoral researchers in the lab, Ben Freedman, now an assistant professor at Harvard Medical School, and Jianyu Li, now an associate professor at McGill, helped use that observation to create medical adhesives now approaching clinical trials (see “A Dressing That Pulls Wounds Shut,” harvardmag.com/mooney-wounds-healing-19). “A lot of really interesting things came about because people in the lab were just observing, thinking,” Mooney says. “Not just about what they were originally intending to do, but taking what came to them and thinking about its implications.”
The strategy seems to come naturally to him. Over and over again, he has immersed himself in a new field—cell biology, immunology, cancer chemotherapy—and emerged with a set of concrete ways to achieve striking breakthroughs.
“He’s really good at taking pie-in-the-sky ideas and distilling them down into manageable chunks,” says Kwasi Adu-Berchie, a Wyss Institute scientist who did his doctoral work in Mooney’s lab. Case in point: with his guidance, Adu-Berchie is working on a vaccine for malaria consisting of an injectable gel loaded with proteins that reshape the body’s immune response to infection. This approach to some of the most difficult problems in medicine—melding a finely tuned sense of the physical world with a deep understanding of biology—is Mooney’s signature, an attitude and an approach to research he hopes to pass on to those who work with him. It has led him to some surprising places.
When he was growing up in Madison, Wisconsin, Mooney didn’t know anyone who was an engineer or scientist—or a professional of any kind. His father, a meter reader at the utility company, also took part-time janitorial jobs to make ends meet, and Mooney remembers helping to empty ashtrays at one of those cleaning gigs. But his parents, whose own parents’ schooling had ended with eighth grade, believed in education for their 11 children. Many of the siblings went to community college and then to university, and went on to careers such as social work, but when Mooney was a freshman at the University of Wisconsin, Madison, an adviser suggested he major in chemical engineering. He’d done well in chemistry and in math, and would be able to get a good job after graduation. Without knowing much more than that, Mooney agreed.
As he worked his way through college, alternating semesters in class with semesters at a job, he learned how to be a chemical engineer through practical experience. He’d arrive at a company, be given a problem that needed solving, and come up with solutions. He liked the work. And one day, when he was asked to scale up the manufacture of a drug molecule for a clinical trial, he realized something: “I could use all this engineering that I was learning…and instead of using it to produce some mass-commodity chemical a dollar cheaper a barrel, I could use it to do something that would help people directly.”
When he arrived in Boston in the late 1980s to begin graduate school at MIT, he worked with biomedical engineer Robert Langer and Homans Distinguished Professor of Surgery Joseph Vacanti, two researchers who were laying the groundwork for what is now called tissue engineering. With the right scaffolding, they thought, cells could be persuaded to grow into things like blood vessels and heart muscle outside the body, ready for transplantation. Mooney was fascinated. Working with them and with Donald Ingber at Boston Children’s Hospital, studying how scaffolding shaped the differentiation of liver cells, he got a taste for finding and solving interesting problems. When he was offered junior faculty posts while completing his doctorate, he hesitated. It felt risky—he was married, with a young son, and though he knew he could succeed at a company, academia seemed uncertain. But eventually, after two post-doctoral years, he was offered a position at University of Michigan and decided to take it.
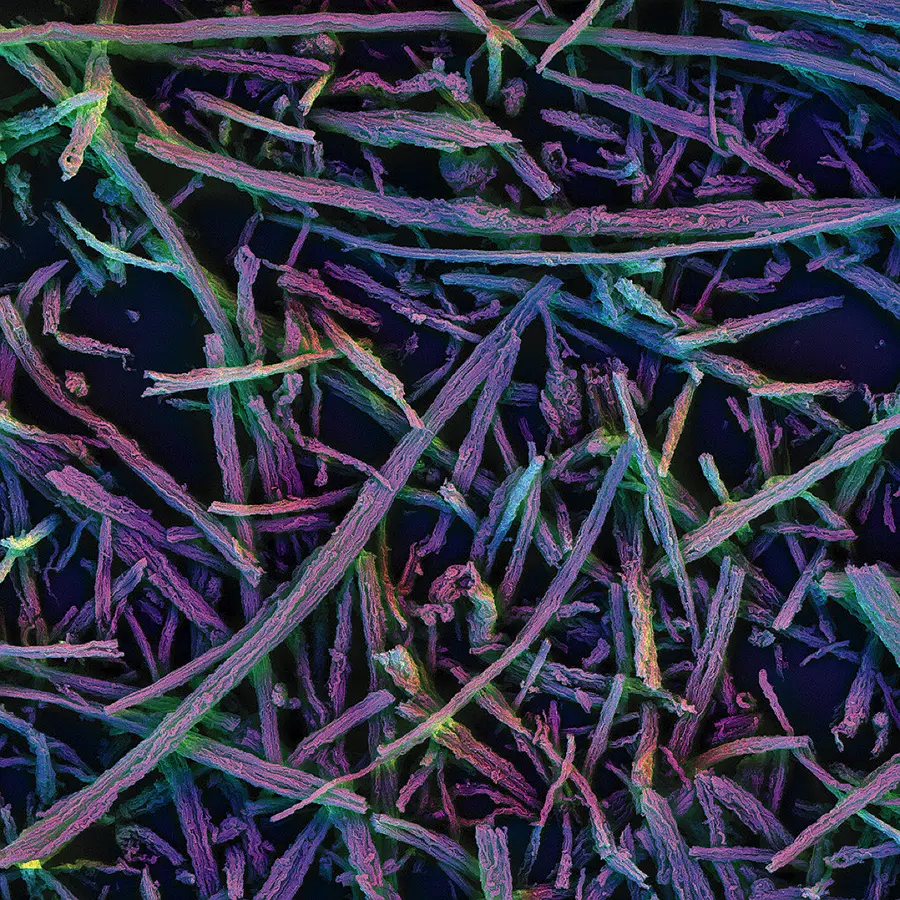
From the beginning, Mooney designed his lab program to ensure that he and his students were never limited to working toward any single goal. He wanted to pursue whatever seemed most intellectually and medically rewarding. The approach soon bore fruit. His research group discovered that in order for scaffold-grown tissue to develop blood vessels successfully, the scaffold itself needed to be imbued with timed-release chemical signals that stabilized the proliferating vascular network. (The approach is now being developed by a company that helps patients with peripheral artery disease, in which blood vessels in the arms and legs narrow.) For a decade, the Mooney lab delved deeply into how gel materials could be engineered to deliver drugs and other substances in precise, skillfully tuned ways, producing paper after highly cited paper. Mooney was becoming a pioneer in the burgeoning field of bioengineering.
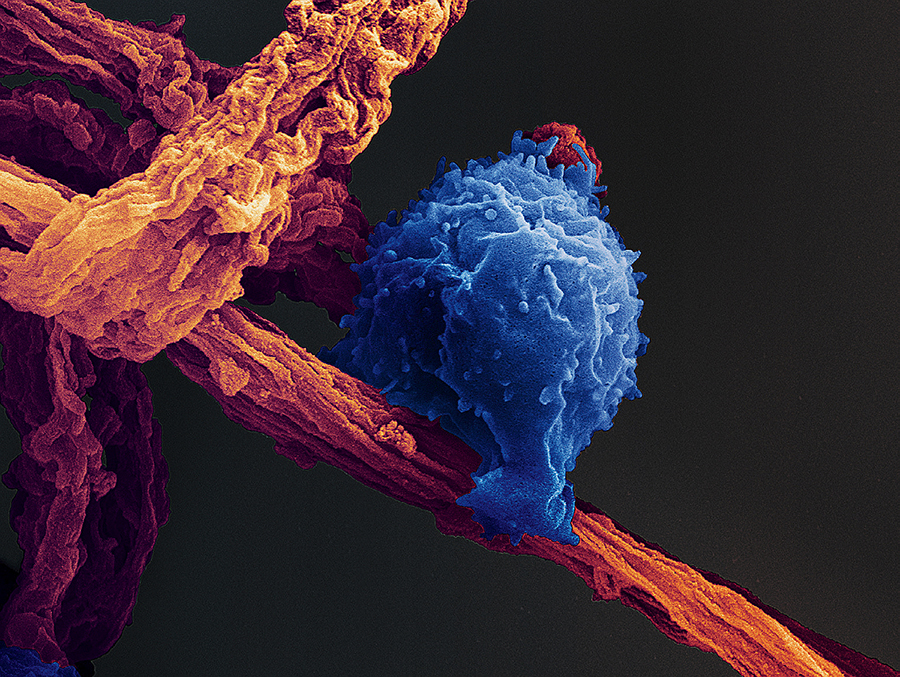
In the process, he realized something that shaped the next couple of decades of his career. Tissue-engineering researchers constantly confronted the problem of inflammation, as immune cells flooded transplant sites, triggering swelling and increased blood flow. One day, Mooney made a telling connection: in a process like vaccination, recruiting immune cells is a feature, not a bug.
Recruiting cells meshed with another idea he’d been mulling. Thinking about the difficulty of programming cells in a lab dish to do what he wanted once he transferred them to a body, he’d wondered about skipping the dish altogether. “Maybe what we could do is move all the biology into the body—in essence, create cell factories inside the human body,” he says. Bioengineered materials, which reliably attracted immune cells’ attention, could bring cells in—and such “factories” could then alter the differentiation of these cells. When he arrived at Harvard in 2004, he set about proving this idea.
Within the discs were lures to draw the immune cells in, boosters to increase immune cell production, and even tissue drawn from the melanoma itself, to teach immune cells what to attack.
Just five years later, a full-fledged test of Mooney’s idea cured mice of melanoma. The devastating skin cancer was already well advanced when the researchers treated some of the mice with a therapeutic vaccine (meant to treat an established disease rather than prevent it). They inserted discs of an engineered polymer about the size of a fingernail, laced with molecules that draw in immune cells, under the skin of treated mice. Within the discs were lures to draw the immune cells in, boosters to increase immune cell production, and even tissue drawn from the melanoma itself, to teach immune cells what to attack. In a little more than three weeks, all the untreated mice were dead, but the vaccinated animals had survival rates of up to 90 percent, depending on their dosage. Very large tumors had melted away under the immune system’s attack. In 2013, the Dana-Farber Cancer Institute (DFCI) enrolled melanoma patients for a clinical trial to test the vaccine Mooney and colleagues had developed in mice. Although the pandemic delayed publication of the results for many years, pharmaceutical company Novartis has nonetheless licensed the technology to begin developing its own vaccines.
Mooney, meanwhile, had become instrumental in founding the Wyss Institute (see harvardmag.com/wyss-gift-19). A meeting with Harvard’s provost soon after Mooney’s arrival emphasized the University’s ambition for a new enterprise focused on bioengineering, one reason for Mooney’s hiring. Mooney agreed to help and suggested bringing on his former graduate-school mentor, Don Ingber, to cochair the committee working on the idea, and Ingber became the founding director of a stand-alone translational research and licensing organization, a position the Folkman professor of vascular engineering still holds. A $125-million gift from Hansjörg Wyss launched the Institute in 2009, with the goal of accelerating the translation of science from labs across Harvard to industry and the clinic. (Since then, with $606 million in further gifts from Wyss, the Institute has become a biotechnology powerhouse, with more than 4,000 patents filed and more than 60 start-up companies launched by its affiliated faculty.)
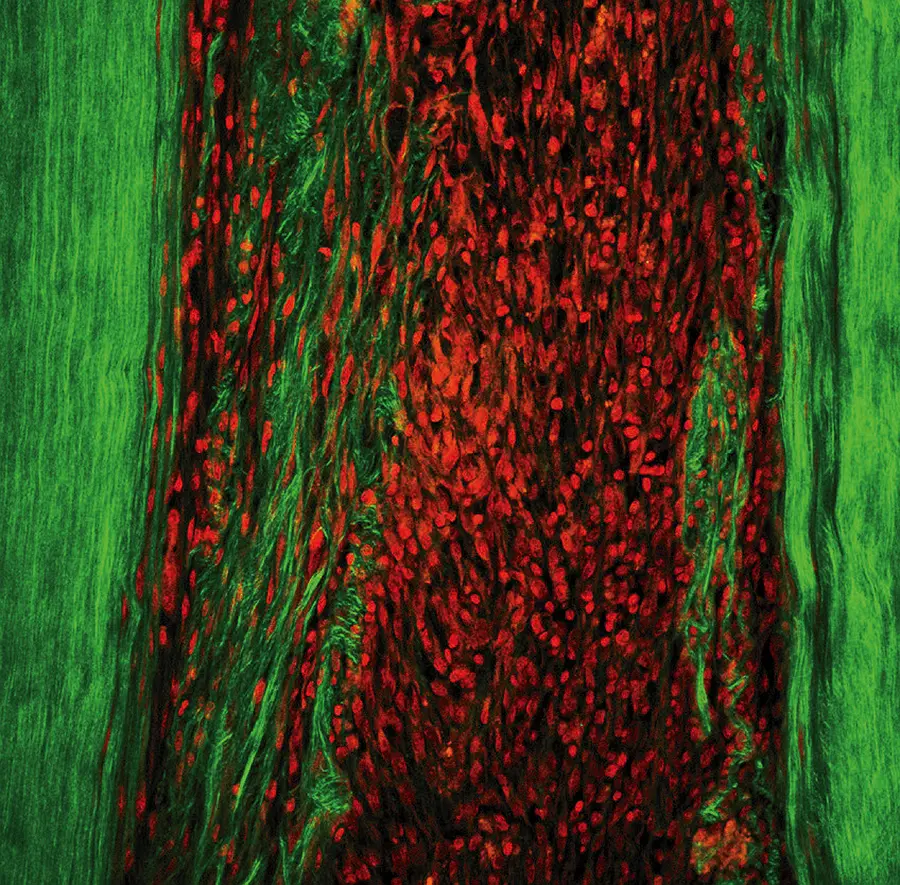
Mooney and his colleagues have continued refining the strategy at the heart of their melanoma vaccine, designing biochemical lures for cells and testing different molecules that can influence and educate them once they arrive in the “factory.” “He’s taken the idea on and on,” says Jeffrey Hubbell, a professor of tissue engineering at the University of Chicago who has watched Mooney’s career with interest. The cancer vaccine was the first tangible result, but now Mooney and his colleagues are creating factories for other purposes. In June 2024, the lab published a method for injecting a biomaterial under the skin that can lure in worn-out CAR T-cells (engineered immune cells that hunt down cancer) and rejuvenate them, with the aim of helping people remain cancer-free longer.
They are expanding the technique to other diseases, as in Adu-Berchie’s malaria vaccine. Malaria, caused by single-celled parasites spread by mosquitoes, is a pitiless adversary—it kills more than half a million people each year, most of them children (see “An Evolving Foe,” March-April 2010, page 42). Last year, a clinical trial of a malaria vaccine in Burkina Faso showed encouraging results, keeping more than 75 percent of recipients healthy. But the vaccine had to be administered in four separate doses spread out over a period of months—a regime that poses a major obstacle for people in rural areas in Africa, who may have to travel long distances to reach treatment centers.
Adu-Berchie, who is from Ghana, was already studying how to use biomaterials in medical treatment, and was familiar with the problem of getting care to under-resourced areas in Africa. Then the Gates Foundation learned about the technologies and reached out to the Mooney lab, wondering if the materials could be used to reduce the number of shots required. He is now working on a biomaterial that could be injected once, under the skin or in the muscle, instead. It could then educate immune cells to identify and attack malaria parasites over a period of weeks or months.
Mooney has even begun to explore how the physical forces exerted on an immune cell—whether it’s in a gel, a fluid, or something in between—can change its ultimate role in the body. T cells have many different jobs, depending on their specific type, including remembering previous infection so the immune system can leap into action when the same pathogen is spotted, chasing down and destroying the invaders. Last year, he, Adu-Berchie, graduate student Yutong Liu, and colleagues found that simply changing the viscosity of the medium in which nascent T cells are grown could control what type of T cell the nascent cells would become. He is also exploring how to increase dramatically the number of cells that can mature into T cells, with an eye toward boosting responses in immunocompromised individuals.
If Mooney has avoided locking himself into a single research goal for his lab, he has a very clear goal for the people within it. “In my mind, there are two types of academic labs,” he says. “There are mission-oriented labs, where basically their mission is to do something specific, cure a disease, understand a molecular pathway. Then there are labs where the main product is not the papers or the discoveries. It’s actually the people.”
Mooney moves and speaks with a kind of spare economy. He is reserved but far from shy. When you talk to him you have the sense that he is committing everything you say to memory, and could, without too much trouble, transmit it back to you a couple of months later. For much of his early career, Mooney let others license his discoveries rather than pursue them himself—an unusual choice for an engineering professor—because he wanted to focus on being present for his young family and mentoring his students. He’s the kind of dad, Don Ingber relates, who builds an ice rink in the backyard to play hockey with his kids, who takes them camping and teaches them about the outdoors. And today, his lab includes nearly 40 people. He meets with each graduate student and post-doc for an hour every two weeks.
His students and post-docs have responded to that attention. Nearly 80 lab alumni came to a birthday symposium planned for Mooney in November, says Ben Freedman, now a cofounder with Mooney of a company commercializing their medical adhesive, Limax Biosciences. Adu-Berchie reflects that almost everyone mentored by Mooney aspires to treat their future students the same way. Freedman himself says, “I miss working with him closely. If I could have worked with Dave in his lab forever, I would have in a heartbeat.”
Mooney also teaches undergraduates and has particular fondness for his engineering and problem-solving class, a small advanced seminar in which students work on real problems for Harvard institutions. Clients have included the Global Health Initiative at DFCI and Boston Children’s Hospital, where the goal was to address the disparity in outcomes of pediatric cancers in developing countries, and the Harvard Stem Cell Institute iPS Core Facility, for which students were tasked with improving the manufacture of stem cells. Each time he teaches the course, he says, there always comes a moment when students realize that if they simply repeat what they’ve learned, without creating something new, they’re missing the point: “How I measure success in this class is [whether] you actually deliver something to your client that they can use.” The process can be extremely rewarding for both the instructor and the students.
Ingber, who has known him a long, long time now, says Mooney’s style as a scientist and leader sets him apart. He has met many big personalities, people whose brilliance is of a showier quality. Mooney—highly intelligent, focused, and compassionate—is a different breed. “People love working with him,” he says. “He is a down-to-earth doer.”
That passion and ingenuity are poised to continue contributing directly to medicine. Translating fundamental science—from immunology to the chemistry of gels—into advances in the clinic, with a minimum of delay, is a key part of the Mooney lab’s ethos. “I don’t think science should just be doing the science and publishing it,” says Adu-Berchie. “Dave has a similar opinion.” Mooney is always thinking about how to apply what he’s found to improve the world, one set of cells at a time. Someday his tiny factories may be working within people around the globe, teaching the body to fight off disease, defend itself from cancer, and perform other feats as yet undreamed of.